I knew the coping skills.
Breathe. Ground. Tap. Text someone. HALT check. Step outside. Name five things you see. Ride the wave. Let the feeling pass.
I could run the playbook in my sleep—and honestly, for a while, it worked.
I stayed sober for more than 90 days. I stayed connected. I stayed functional. I even helped others in the program when they felt overwhelmed.
But here’s what no one tells you: you can be doing “everything right,” and still feel like something’s crawling under your skin. You can stay sober and still feel like you’re about to explode.
That’s where I was. And that’s why I needed something deeper.
That’s why I turned to EMDR.
I Was Managing My Symptoms, Not Healing My Triggers
Let me say this clearly: I don’t regret learning coping skills. They saved my life. They gave me a way to stay afloat.
But after a while, I didn’t want to just manage. I wanted peace. I wanted space in my body that didn’t feel like panic. I wanted to go to a party and not feel like I was faking it. I wanted to stop obsessing every time I got a text that said “We need to talk.”
I wanted to stop rehearsing my trauma responses in my head just in case something went wrong.
The more I stayed sober, the more I realized that emotional triggers weren’t getting better—they were just getting quieter. But they were still running the show.
And eventually, that inner pressure made me slip. Not once. Twice.
My Slips Weren’t About “Willpower”
After my second relapse, I sat across from my sponsor and couldn’t stop crying. Not out of guilt, but out of exhaustion. I was tired of trying so hard. Tired of white-knuckling my way through everything that reminded me of the past.
And she looked at me and said something I’ll never forget:
“You don’t need another checklist. You need something that goes where the fear lives.”
She recommended EMDR. I’d heard of it before—mostly in trauma circles—but I never thought it applied to me. I didn’t have some huge, violent trauma. My pain was quieter. Lonelier. Slower.
But as I started to learn more, I realized that’s exactly the kind of pain EMDR can reach.
What Is EMDR, Really?
EMDR stands for Eye Movement Desensitization and Reprocessing. It’s a therapy technique that helps people reprocess memories that get stuck in the brain—memories that didn’t finish “processing” the normal way because they were overwhelming or threatening at the time.
It’s not talk therapy, exactly. You don’t need to tell the full story. You focus on key moments—the ones your body still reacts to—and use bilateral stimulation (like eye movements or tapping) while holding those memories in mind.
Somehow—and I still don’t fully get the science—it takes the sting out. It separates the memory from the panic. It helps your brain realize: This already happened. It’s not happening now.
At Greater Boston Behavioral Health, I found a therapist who specialized in EMDR for people in recovery. That mattered to me. She didn’t flinch when I mentioned relapse. She didn’t moralize. She just said, “Let’s figure out what your body still thinks it has to survive.”
That changed everything.
It Wasn’t Dramatic—But It Was Deep
I thought EMDR would be intense and fast. Some sessions were. But a lot of it was gentle. Thoughtful. We didn’t start with the worst memory. We started with what my brain kept looping—tiny moments with huge meaning.
Like a birthday where no one showed up. A moment where someone I trusted rolled their eyes. A breakup where I begged someone to stay, even though they were already gone.
These weren’t “headline traumas.” But they shaped how I saw myself.
I wasn’t lovable. I wasn’t safe. I couldn’t be soft.
In EMDR, I revisited those memories—not to relive them, but to let my nervous system complete the story.
And when I say things shifted, I mean it. I stopped bracing for rejection in every interaction. I stopped needing people to “prove” they cared. I started feeling more in myself—not just performing recovery, but experiencing it.
I Still Use My Tools—But I Don’t Live in Hypervigilance
Don’t get me wrong, I still journal. I still meditate. I still check in. But I no longer need to coach myself through every moment of discomfort.
EMDR didn’t make me immune to pain. But it made me less allergic to it.
I can feel sadness without assuming it will drown me. I can feel loneliness without thinking I have to fix it with a substance or a distraction. I can have hard conversations without shaking or shutting down.
And that? That’s freedom I didn’t know I was allowed to have.
If You’ve Relapsed After Doing “Everything Right”—You’re Not Broken
I used to think relapse meant failure. That I didn’t work hard enough. That I didn’t want it badly enough.
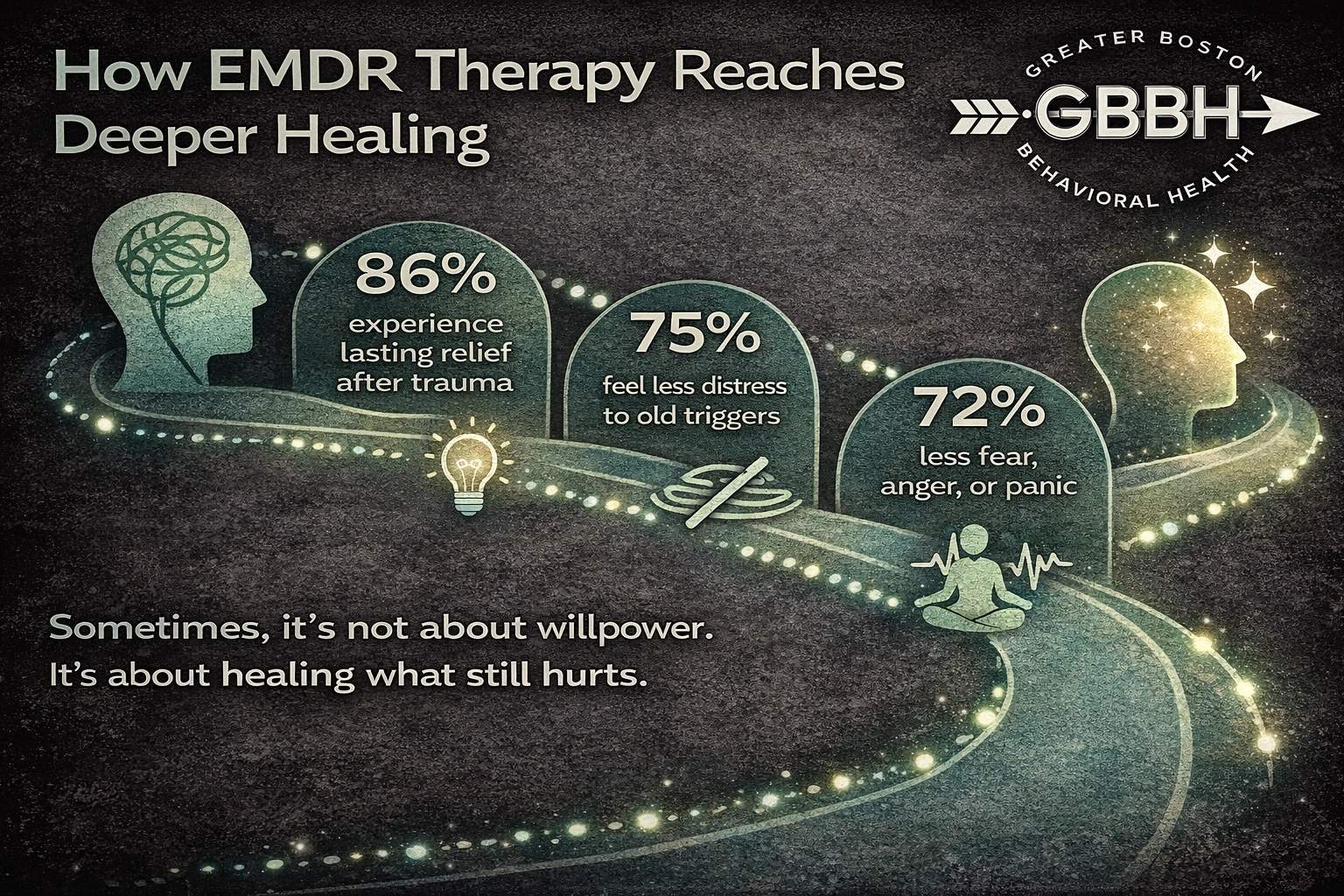
Now I understand: coping can’t always heal what trauma created.
If your nervous system still thinks the danger is here, no amount of logic will override it. EMDR helped me stop living like every disappointment was a threat. It helped me take up space again.
I’m not perfect. I still have rough days. But I haven’t relapsed since EMDR—and it’s not because I’m stronger. It’s because I’m safer in my own mind.
EMDR Services Available Near You
If this resonates—even a little—know that help is close. At Greater Boston Behavioral Health, we offer trauma-informed EMDR therapy for people navigating recovery, relapse, or emotional triggers that won’t loosen their grip.
Whether you’re based in the city or searching for EMDR in Newton, MA, you’re not far from clinicians who understand that relapse isn’t the whole story—and that healing doesn’t end with sobriety.
Frequently Asked Questions (FAQs)
What does EMDR actually do?
EMDR helps your brain reprocess traumatic or distressing memories so they no longer trigger intense emotional or physical reactions. It separates the memory from the fight-or-flight response.
Is EMDR just for people with PTSD?
No. EMDR is effective for a wide range of experiences—childhood neglect, bullying, emotional abuse, complicated grief, or any stuck emotional patterns. It’s often used in recovery when triggers remain even after sobriety.
How long does EMDR take to work?
Some people feel shifts within a few sessions. Others need more time. It depends on your goals and the intensity of what you’re processing. Your therapist will pace it with you.
Do I have to talk about every detail of my trauma?
No. That’s one of the unique parts of EMDR—you can keep the details private and still experience healing. It works on how the memory is stored, not just what you say about it.
Will it feel overwhelming?
It can be emotional, yes. But sessions are structured and supported. You won’t be “left in it.” A good EMDR therapist will guide you in and out of the work safely.
You Deserve More Than “Getting By”
You don’t have to wait for another breakdown. You don’t have to prove you’re “sick enough.” You don’t have to go back to square one.
You just have to ask yourself one question: What if there’s more healing available than I thought?
Call (888) 450-3097 to learn more about our EMDR services in Boston, Massachusetts.