I used to think help was for other people.
Not people like me. Not someone who had a job, paid their bills, showed up, and looked fine.
I wasn’t the person who’d “hit bottom.” I wasn’t sleeping on park benches or waking up in strange places. I hadn’t lost my job. I hadn’t lost my relationships.
But I had lost something else—myself.
I was functioning on the outside, but slowly unraveling inside. Numbing with alcohol. Overworking. Avoiding everything that hurt. I could talk to anyone—but I wasn’t telling the truth to myself.
And still, for too long, I told myself I wasn’t “sick enough” to need help.
It took me almost falling apart in silence to realize I didn’t have to.
That’s how I ended up in an Intensive Outpatient Program in Boston—and how it quietly saved my life.
The Dangerous Lie: “I’m Fine”
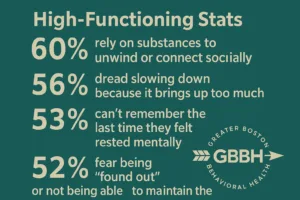
There’s a special kind of trap for people who function well: you start believing your performance means your pain doesn’t count.
For me, it looked like this:
- Morning coffees masking hangovers
- Telling myself I was “taking the edge off” every night
- Saying yes to everything while resenting everyone
- Feeling emotionally absent from my own life
- Constantly on guard so no one would know how bad it really was
I had everything people told me would make me happy. But none of it felt real.
I kept saying I was “fine” because admitting otherwise felt like weakness. I didn’t fit the stereotype of someone who needed a program. But I needed help—desperately.
My Breaking Point Was Invisible
The night I realized something had to change, nothing dramatic happened.
No car crash. No public meltdown. Just a regular evening, me alone on the couch, finishing a bottle of wine I told myself I’d only have a glass from.
I remember thinking: I’m not even getting drunk anymore. I’m just trying to feel normal.
I Googled “Intensive Outpatient Program Boston” that night, fully expecting to talk myself out of it the next morning.
But I didn’t. Because something in me knew this wasn’t sustainable anymore.
IOP Didn’t Judge Me—It Met Me
I called Greater Boston Behavioral Health the next day. Shaky, ashamed, and half-expecting a lecture.
Instead, I got a real human voice. Calm. Warm. Asking questions, not assumptions.
No one demanded I label myself. No one asked me to start with my “worst moment.” They just listened.
I got to say the quiet part out loud: I don’t know if I belong here, but I can’t keep living like this.
That was enough. And it turned out, I wasn’t alone.
Who I Found in the Room Surprised Me
I expected IOP to feel clinical or cold. I thought everyone would have a tragic story worse than mine. I worried I’d feel like an imposter.
But that first week?
I met people who looked just like me. A nurse. A mom. A teacher. A guy who ran marathons and drank himself to sleep. A woman who hadn’t smiled in six months.
Nobody fit the stereotype. But everyone was there for the same reason: they couldn’t keep pretending things were okay when they weren’t.
We weren’t broken. We were burned out. Buried under expectations. Using whatever we could to stay afloat.
IOP Didn’t Shame Me Into Healing—It Gave Me Tools to Try
I didn’t need someone to “fix” me. I needed someone to help me stop lying to myself. And that’s exactly what IOP did.
It taught me how to:
- Understand my triggers instead of denying them
- Set real boundaries without guilt
- Stop defaulting to wine, weed, or work to cope
- Build routines that support—not punish—my mental health
- Feel my feelings without drowning in them
The structure helped. So did the community. So did knowing I could walk into a space three to five times a week and not have to pretend.
I kept working. I kept paying bills. I kept showing up for my life. But I started doing it from a place of honesty, not exhaustion.
What Made IOP Different From Therapy
I’d been in therapy before. It helped—but it wasn’t enough.
What IOP gave me that therapy didn’t:
- Frequency: Multiple sessions a week meant I didn’t spiral between appointments.
- Accountability: I had people checking in who cared whether I showed up.
- Integration: I could apply what I was learning in real time.
- Community healing: Being with others who “got it” changed everything.
Even if you’re looking for an Intensive Outpatient Program in Wellesley, MA, Newton, or Dedham—there’s a version of this that works around your life.
This wasn’t about checking out of life. It was about learning to live differently within it.
IOP Wasn’t My Rock Bottom—It Was My Turning Point
I didn’t lose everything. I didn’t get a diagnosis that shocked me into change.
I just got tired. Of pretending. Of over-functioning. Of using wine to numb and ambition to distract.
IOP was the first space where I didn’t have to explain myself. I didn’t have to perform. I just had to show up, exactly as I was.
And showing up—when I had every reason not to—is what saved me.
What I Know Now (That I Wish I’d Known Then)
If you’re reading this and wondering if you’re “bad enough” to need help—you’re asking the wrong question.
The real question is: Are you living the way you want to live?
If the answer is no, then you deserve support. You deserve clarity. You deserve peace that doesn’t come from a bottle, a binge, or a packed calendar.
Whether you’re in Boston or looking for an Intensive Outpatient Program in Waltham, MA, you don’t have to keep managing alone.
FAQs: For the Person Who’s Still Not Sure
I don’t drink every day. Do I really need an IOP?
It’s not about frequency—it’s about function. If your use is getting in the way of your life or your mental health, that’s enough to explore IOP.
Will I have to stop working?
Not at all. IOP at GB Behavioral Health is designed to fit around work schedules with daytime and evening options.
What if I don’t relate to “addiction language”?
Same. I didn’t call myself an addict, and I was still welcomed fully. You can engage without labels.
What happens after IOP ends?
You’ll work with the team on a plan—individual therapy, support groups, or step-down services. You’re not cut loose. You’re supported as you transition.
Is it weird to be in group therapy?
At first, maybe. But it becomes a relief. You realize you’re not the only one who’s been hiding in plain sight.
If You See Yourself Here, It’s Time
You don’t have to break down to ask for help. You just have to be ready to stop pretending.
There’s no medal for struggling alone.
Call (888) 450-3097 to learn more about Intensive Outpatient Program in Boston, Massachusetts.
If you’re high-functioning, high-achieving, and quietly hurting—you’re not alone. You’re not too late. You’re right on time.