You stopped going.
Maybe it was after a rough session. Maybe it started as “just a couple missed days.” Maybe you ghosted hard—no warning, no follow-up, just vanished.
Now here you are—considering walking back into your intensive outpatient program—and your brain is loud about it.
What if they’re mad I left?
What if everyone judges me?
What if I blew my one shot at getting better?
If that’s what you’re carrying, take a breath. You’re not the only one who’s ever left—and you’re definitely not the only one wondering if it’s “too late” to come back.
Spoiler: It’s not too late. And you’re allowed to return without shame.
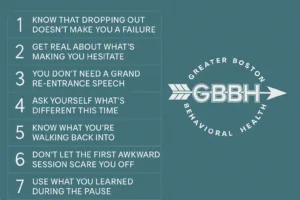
Step 1: Know That Dropping Out Doesn’t Make You a Failure
Let’s start here because shame loves to shout first.
You’re not weak for leaving. You’re human.
Sometimes people pause treatment because life gets chaotic. Sometimes it’s money. Or burnout. Or fear. Sometimes the pain you’re trying to heal feels too overwhelming, and you hit the eject button.
Guess what? That doesn’t erase the work you did do.
And it doesn’t mean you don’t deserve to return.
Whether you left three days ago or three months ago, that door didn’t close behind you. Most IOP teams—including ours—expect clients to fall off sometimes. And we keep the light on anyway.
Step 2: Get Real About What’s Making You Hesitate
What’s holding you back from walking in again?
Is it embarrassment?
Fear you’ll have to explain yourself?
Worry that you’ll feel “behind” or like the new kid again?
None of that is silly. It’s real. But here’s the thing—those fears are usually louder than reality.
In most intensive outpatient programs, people cycle in and out all the time. Staff members understand what it means to struggle, stall, and restart. They don’t expect perfection.
And the other clients? They’re focused on surviving their own battles—not keeping score on yours.
Step 3: You Don’t Need a Grand Re-Entrance Speech
Seriously. You don’t need to walk in and pour out some emotional TED Talk.
If you want to say something, keep it simple:
- “I’m back.”
- “Things got hard—I needed time.”
- “Can I restart?”
You can speak from the heart—or not. You can write it down. You can even say nothing and just show up.
We promise, there’s no welcome-back quiz.
What matters is that you show up. That alone is a statement.
Step 4: Ask Yourself What’s Different This Time
Maybe the pain got louder.
Maybe the support ran thin.
Maybe you’ve finally had enough of pretending you’re okay when you’re not.
Whatever brought you back to this page, that “something” matters.
You don’t have to come back knowing exactly how things will go. But knowing what made you reconsider returning? That’s a good place to begin.
Use it as your anchor when things get hard again. And they might. But you’ll be grounded differently this time.
Step 5: Know What You’re Walking Back Into
An intensive outpatient program isn’t jail. It’s not a lecture hall. And it’s not a courtroom waiting to deliver a verdict on how “committed” you are.
At Greater Boston Behavioral Health, our IOP is structured—but human. That means:
- You’ll have scheduled sessions and groups.
- You’ll work with professionals who are trauma-informed and recovery-experienced.
- You’ll be treated like a person, not a project.
We don’t reopen your file with side-eye. We open it with hope that maybe this time, it’ll click better. Because maybe you are different now.
If you’re in Newton, Dedham, or Needham, MA, we’ve got local programs that honor second chances—and third and fourth ones, too.
Step 6: Don’t Let the First Awkward Session Scare You Off
The first day back might feel weird. That’s okay.
You might feel self-conscious, overly aware of who’s in the room. You might catch yourself wondering what they’re thinking. You might be tempted to leave at the first break.
That’s the moment to breathe. Stay. Sit through the awkward.
Because here’s the quiet truth: most people in the room are thinking, “I’m glad they came back.”
They get it. They’ve been it.
Step 7: Use What You Learned During the Pause
You didn’t just “lose progress.” You learned something.
Maybe you discovered what doesn’t work. Maybe you hit a limit. Maybe life on the outside got too loud.
That’s data. And data = power.
Use what you learned while you were away to shape this next stretch of healing. What do you need more of? Less of? Different support around?
You’re not starting over. You’re resuming—with new wisdom.
Step 8: Believe That This Can Still Work for You
You might feel like you already “blew it.” That the help only works if you never leave. That maybe it’s too late to try again.
None of that’s true.
Success in IOP isn’t about never falling—it’s about knowing how to get up.
Every time you return, your chances of healing get stronger. Because you’re building resilience. Because you’re learning your patterns. Because you’re still in the fight.
And trust us—your fight is worth it.
FAQs: What to Know About Returning to IOP
Q: Is it normal to leave and come back to IOP?
Yes. Life happens. Motivation shifts. Emotions get overwhelming. Returning after a break is common—and respected. You’re not “failing” by coming back. You’re recommitting.
Q: Will I have to start completely over?
Not usually. Your care team will reassess with you and create a plan based on where you are now. Some clients continue where they left off. Others make adjustments. It’s flexible and personalized.
Q: What if I’m embarrassed to face the group or staff?
That’s understandable—but you’ll likely be surprised by how supportive people are. Many clients have been through the same thing. And staff? They’re just glad you’re safe and willing to re-engage.
Q: Do I need a referral or special permission to return?
Not typically. Just call the program or reach out via email to express that you’d like to rejoin. The admissions or clinical team will guide you from there.
Q: What makes Greater Boston Behavioral Health’s IOP different?
We understand the emotional reality of re-entry. You won’t be met with shame or bureaucracy—we offer structured, trauma-informed IOP care in Boston and surrounding areas. And we mean it when we say: the door is still open.
You Didn’t Miss Your Shot—You Just Paused
If you’ve been beating yourself up for leaving, consider this your permission to stop. You didn’t ruin your chances. You didn’t “waste” the opportunity. You’re not behind. You’re human.
Coming back doesn’t make you weak. It makes you brave. And healing? Healing is always on the table—even when you’ve stepped away from it before.
Call (888) 450-3097 to learn more about our intensive outpatient program services in Boston, Massachusetts. There’s still room for you here. Let this be your return. We’re ready when you are.