You stopped going. Maybe without warning. Maybe with every intention of coming back.
You told yourself it was just a break. You’d been working hard. Maybe too hard. You were tired of talking, tired of feeling, tired of staring at the screen or walking into another group circle, pretending to be okay when you weren’t even sure what that meant anymore.
You didn’t plan to ghost your intensive outpatient program. But here you are. And now there’s this quiet, nagging voice asking, Was that a reset… or the beginning of a slide?
If you’re here reading this, you’re already doing the bravest thing: you’re checking in with yourself.
Let’s walk through it together.
1. Check: Why Did You Leave?
Not the surface-level reason. Not the “I was busy” or “it wasn’t helping.”
Underneath that—what was going on?
- Did therapy feel too intense too fast?
- Did a tough session trigger something you weren’t ready to face?
- Were you feeling okay and wanted space to see if you could manage solo?
- Were you quietly sliding back into avoidance or old habits?
Whatever the answer is, you’re allowed to name it. Leaving doesn’t mean you failed. It just means something shifted—and it’s worth being honest about what.
2. What’s Changed Since You Left?
One of the clearest ways to know if your break is healthy or harmful is to look at the aftermath.
Are you more regulated?
Sleeping better?
Taking care of things you couldn’t before?
Or…
Have you stopped responding to texts?
Is your mind foggier, heavier, darker than it was?
Have old patterns come creeping back in—slowly, quietly, with no fanfare?
Relapse isn’t always dramatic. Sometimes it’s as subtle as skipping a meal. Ignoring a call. Telling yourself you’ll rejoin tomorrow—again.
3. Be Honest About the Difference Between Rest and Numbing
There’s a big difference between needing rest and falling back into numbing.
Rest feels like:
- Breathing easier
- Reconnecting with real life
- Getting clearer, steadier
Numbing feels like:
- Over-scrolling, over-sleeping, over-avoiding
- Losing track of time
- Hiding how you’re really doing
Only you know what this break has felt like. But if it’s starting to feel more like avoidance than recovery… it might be time to check back in.
4. Ask Yourself: What Am I Avoiding?
It’s okay if you don’t want to go back. But ask yourself: Why?
Sometimes we step away from IOP because we’re scared of what’s coming up.
The grief.
The guilt.
The stuff that therapy starts to dig up—the parts of your story that were easier to keep buried.
That doesn’t mean you’re not ready. It means you’re human.
Leaving doesn’t erase the work you’ve done. And coming back doesn’t mean starting over. It just means you’re choosing to face what’s real—with help.
5. Look at Who You’re Still in Contact With
One red flag that a break is turning into a slide? Disconnection.
If the people who knew your story—the ones you were honest with in group—haven’t heard from you… that might be a sign something’s off.
Even if you told them you needed time, ask yourself: Why haven’t I checked in?
If your healthiest people don’t know how you’re doing… it might be because you don’t want to say it out loud.
That’s okay. But you don’t have to stay in that place.
6. Notice How You Talk to Yourself
Self-talk tells the truth. Listen to it.
Do you hear:
- “I’ll go back next week, for real this time…”
- “I messed this up.”
- “They probably don’t want me back anyway.”
- “I can’t face them.”
That’s not laziness. That’s shame. And it’s a liar.
We don’t blacklist people for disappearing. We don’t punish dropouts. You’re not being graded. You’re being invited to come back—messy, imperfect, unsure. That’s what we expect.
If you’re looking for an intensive outpatient program in Dedham, MA or nearby, we’ve kept the door open. You still have a seat.
7. Remember What IOP Was Actually Giving You
It’s easy to forget when you’re outside the routine—but IOP wasn’t just “talking about feelings.”
It was:
- Accountability
- Structure
- A reason to get out of bed
- A group of people who knew you beyond your mask
- Tools you may have started learning but haven’t finished building
That’s not nothing. That’s scaffolding. And it’s okay to realize you still need it.
Needing support again isn’t failure. It’s clarity.
8. Ask: “What Would Going Back Actually Look Like?”
It doesn’t have to be all or nothing. You don’t have to re-enter like nothing happened. You don’t even need to know how to come back. That’s our job.
Just ask yourself:
- Could I reach out and have a low-pressure conversation?
- Could I return for one session and see how it feels?
- Could I talk about adjusting my schedule or needs?
A good intensive outpatient program in Boston, MA will meet you where you are—not where they think you “should” be.
FAQ: Rejoining or Restarting IOP After Leaving
Can I come back after ghosting?
Yes. 100%. You’re not disqualified. You’re not blacklisted. We’ve seen it before—and we’re ready to welcome you when you’re ready.
Do I have to explain why I left?
You can if you want, but you’re not obligated to justify your journey. We care more about where you are now than what happened then.
What if I can’t commit to the same schedule again?
That’s okay. Let’s talk. Some people need modified tracks or slower re-entry. Flexibility doesn’t mean you’re taking shortcuts—it means we’re making care sustainable.
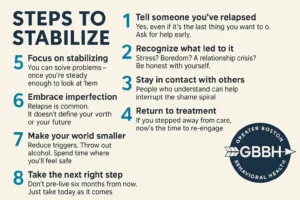
What if I relapse before I reach out?
It’s okay. You’re still welcome. IOP can work alongside other support like detox or residential if needed. But we won’t shame you for slipping. We’ll help you get stable again.
Can I get support without fully re-enrolling?
Sometimes, yes. A re-engagement consult, a check-in, a brief phase return—all possible. Let’s talk through what feels right for this moment.
Thinking about coming back—but not sure how to start?
Call (888) 450-3097 or visit our intensive outpatient program services in Boston, Massachusetts. And for those in Needham, Waltham, Newton, or West Roxbury, we have nearby locations to make care accessible. We’re here to support you—without shame, pressure, or judgment.