There’s a moment in long-term recovery that nobody talks about enough.
It’s not the relapse. It’s not the rock bottom. It’s the flatness.
You’re technically doing well. You haven’t spiraled. You still show up to work. You smile when people make jokes. You don’t have a dramatic “before and after” to post about anymore.
But inside? It’s quiet. Hollow. Like the lights are on but you’re not really home.
That was me. Years into my recovery. And yet, I felt like a stranger to my own progress. The habits were there. The insight was there. But the spark? Gone.
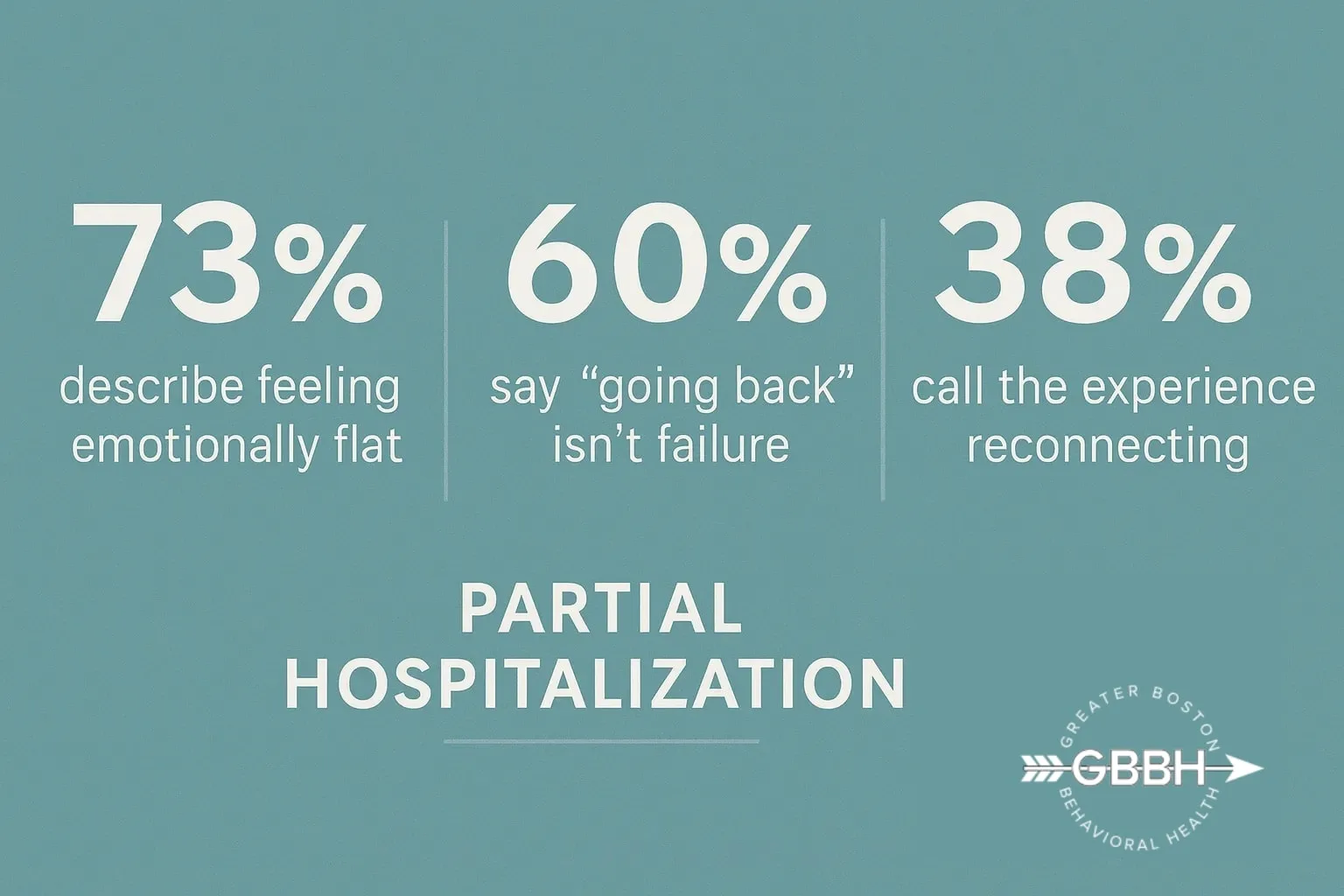
I didn’t want to admit it—not to my therapist, not to my friends, and definitely not to myself—but I was stuck. Not in crisis. Just stuck. Stagnant. And the idea of re-entering a Partial Hospitalization Program (PHP)? That felt like admitting defeat.
But what actually happened when I went back? It changed everything. And it didn’t look anything like failure.
The Numbness Caught Me Off Guard
I wasn’t drowning. That’s what made it so easy to ignore.
I was functioning. I was keeping the house clean, answering emails, paying bills. But every day felt like it was happening two inches away from me. I couldn’t remember the last time I cried—or felt genuinely excited about anything.
In the early days of recovery, my emotions had been intense and alive. Now? I felt emotionally flattened. Like all the color had drained out of life and been replaced by gray.
When I tried to explain it to someone, I said, “It’s like I’m technically alive, but my soul’s on airplane mode.”
I Thought “Going Back” Meant “Starting Over”
I had a pretty harsh internal monologue running when the idea of PHP came up.
“You’ve already done this. You should be past this.”
“People who relapse go back. Not people like you.”
“What are you even going to talk about in group? You’re just… tired.”
But Greater Boston Behavioral Health offered something that cut through that spiral: a reframe.
They said, “This isn’t a setback. It’s a tune-up.”
That language mattered. It gave me permission to look at my exhaustion not as weakness, but as data. And PHP wasn’t a punishment. It was a way to re-engage.
What Returning to PHP Looked Like (Emotionally and Logistically)
When I re-entered the Partial Hospitalization Program in Boston, I expected awkwardness. Embarrassment. I braced myself for sideways glances.
None of that happened.
I was met with welcome. With professionalism. With zero judgment. Most importantly, with clinical respect. They saw me not as a dropout, not as a failure—but as someone self-aware enough to say, “I want to feel more alive than this.”
PHP involved five days a week of structure. Individual therapy. Group therapy. Psychiatric support. Skills-based sessions. A full therapeutic container to explore what had gone flat—and why.
I wasn’t asked to rehash my entire story. I was asked, “Where are you today?” That changed everything.
Group Therapy Wasn’t Repetitive—It Was Deeper
I walked in thinking I’d be the “veteran” in group. The one who’d already “done the work.” I expected to sit in the back and let newer clients take the spotlight.
Instead, I got humbled—in the best way.
Group showed me all the places I’d gotten lazy with myself. The ways I’d built emotional armor. The blind spots I didn’t even know I still had. I saw myself reflected in people 10 years younger who were naming things I’d buried under “functioning just fine.”
That discomfort? It cracked something open. And from there, real reconnection began.
“High-Functioning” Doesn’t Mean Emotionally Well
This hit me hard halfway through week two.
I had been using productivity to cover up emotional stagnation. I wasn’t well—I was just busy. I wasn’t connected—I was performing wellness.
In PHP, I was able to slow down enough to ask questions like:
- What am I numbing by always being in control?
- When did I last feel joy without guilt?
- Who am I outside of being helpful, reliable, and “good”?
That work wasn’t flashy. It didn’t look like early recovery. But it was real.
And it was necessary.
I Didn’t Need Crisis to Justify Care—And Neither Do You
If you’re reading this and thinking, “But I’m not falling apart”—that’s exactly who this blog is for.
You don’t need to crash to return to care. You don’t need to justify your pain by how visible it is.
If you feel:
- Emotionally flat
- Disconnected from your purpose
- Exhausted by “fine”
- Quietly angry at yourself for not being more grateful
Then PHP might be the next right thing—not because you’re broken, but because you want more.
And you deserve more.
Going Back Didn’t Diminish My Growth—It Deepened It
The fear I had going in was that returning to PHP would undo the progress I’d made.
It didn’t. It amplified it.
I came in with more insight. More language. More clarity. That let me go deeper, faster. And I left with not just new tools, but a renewed sense of why I’m still doing this work.
Leaving PHP the first time saved my life.
Coming back saved my spirit.
FAQ: Returning to a Partial Hospitalization Program
Q: Isn’t PHP just for people in acute crisis?
A: Not at all. While PHP can support people in crisis, it’s also used by long-term alumni who are stuck, disconnected, or seeking growth. It’s for anyone who wants structured, intensive care—even without acute symptoms.
Q: Will I have to start from scratch?
A: No. You bring all your progress with you. Our team works with you to build on your insight, not erase it.
Q: What if I feel embarrassed to return?
A: That’s valid—and very common. But no one here sees you as a failure. In fact, returning shows strength, not weakness. We respect your choice to come back.
Q: Can I still work while in PHP?
A: That depends on your schedule and capacity. PHP is a full-day commitment (typically 5 days/week), but some clients adjust their work schedules or take short-term leave. Our team can help you plan that.
Q: How long does PHP last?
A: The length varies. Some people do a few weeks. Others stay longer. The goal is stability and reconnection—not rushing through a set timeline.
Call (888) 450-3097 or visit our Partial Hospitalization Program in Boston, Massachusetts to learn more about your options. Whether you’re deep in disconnect or just starting to ask, “Is this all there is?”—we’re here. Without judgment. Without pressure. With real support.
Going back doesn’t mean you’re failing.
It means you’re still choosing to heal.