I didn’t think I’d be writing something like this.
Ninety days sober. Chips. Applause. The quiet pride of waking up clear-headed. And then… I drank again. Or used again. Or spiraled again. However it happened for you, I know the feeling that comes after.
That hollow drop in your stomach.
That voice that says, “You ruined it.”
What I didn’t know the first time around was that sobriety and healing aren’t always the same thing. And for me, emdr wasn’t part of my first treatment plan.
It is now.
And it’s changing everything.
I Did Everything “Right” The First Time
I showed up. I participated. I followed structure. I learned coping skills and relapse prevention strategies. I could name my triggers. I could call someone instead of isolating.
From the outside, I was doing recovery correctly.
But inside, there were still memories I wouldn’t touch. Conversations I shut down. Images that flashed at night when things got quiet.
I thought that was normal. I thought everyone just carried that stuff and powered through.
The truth? I was building sobriety on top of unprocessed trauma. And trauma has a way of leaking through the cracks.
Relapse Didn’t Mean I Didn’t Care
This part is important.
Relapse doesn’t automatically mean you stopped trying. It doesn’t mean you didn’t learn anything. It doesn’t erase your growth.
For me, relapse felt less like rebellion and more like exhaustion. My nervous system was still stuck in old survival patterns. When stress hit hard enough, my body reached for what it knew would numb it fast.
That doesn’t make it okay. But it makes it understandable.
And understanding changes the conversation from shame to strategy.
What EMDR Actually Does (And Why I Wish I’d Known Sooner)
When I first heard about emdr, I assumed it was just another therapy technique with a complicated name.
It’s not.
Eye Movement Desensitization and Reprocessing is designed to help your brain reprocess traumatic or distressing memories so they no longer feel immediate or overwhelming. Instead of talking about the same event over and over, you work with a trained therapist to activate bilateral stimulation—often through guided eye movements—while focusing on specific memories.
Here’s what that meant for me in real life:
- The memory didn’t disappear.
- I didn’t suddenly “forgive” everything.
- But the emotional charge shifted.
What once felt like a live wire started to feel like a photograph. Still there. Still real. But not electrified.
My body stopped reacting as if the past was happening again.
And when your body isn’t constantly bracing for impact, you don’t need escape in the same way.
Why EMDR Feels Different From Just “Talking It Out”
In my first round of treatment, I could explain my trauma in a calm voice.
I had the story memorized.
But telling the story and healing the story are two different things.
With emdr, the focus wasn’t on intellectual understanding. It was on how the memory was stored in my nervous system.
There were moments in session where I noticed my chest loosen for the first time in years. Moments where an old belief—“I’m not safe” or “This was my fault”—started to shift.
Not because someone argued with me.
But because my brain processed the experience differently.
It’s strange. Subtle. Powerful.
Like watching a knot slowly untangle instead of trying to rip it apart.
Coming Back After 90 Days Is Humbling
If you’re an alum who relapsed after 90 days or more, you know the specific kind of humility that brings.
You’re not brand new.
You’re not clueless.
You know the language. You know the tools.
And that can make it harder.
You might think, “I should know better.”
You might avoid reaching out because you’re embarrassed.
I almost didn’t come back.
What helped me was remembering this: relapse doesn’t mean the first treatment failed. It might mean it addressed one layer, and now you’re ready for the next.
For some of us, that next layer is trauma work.
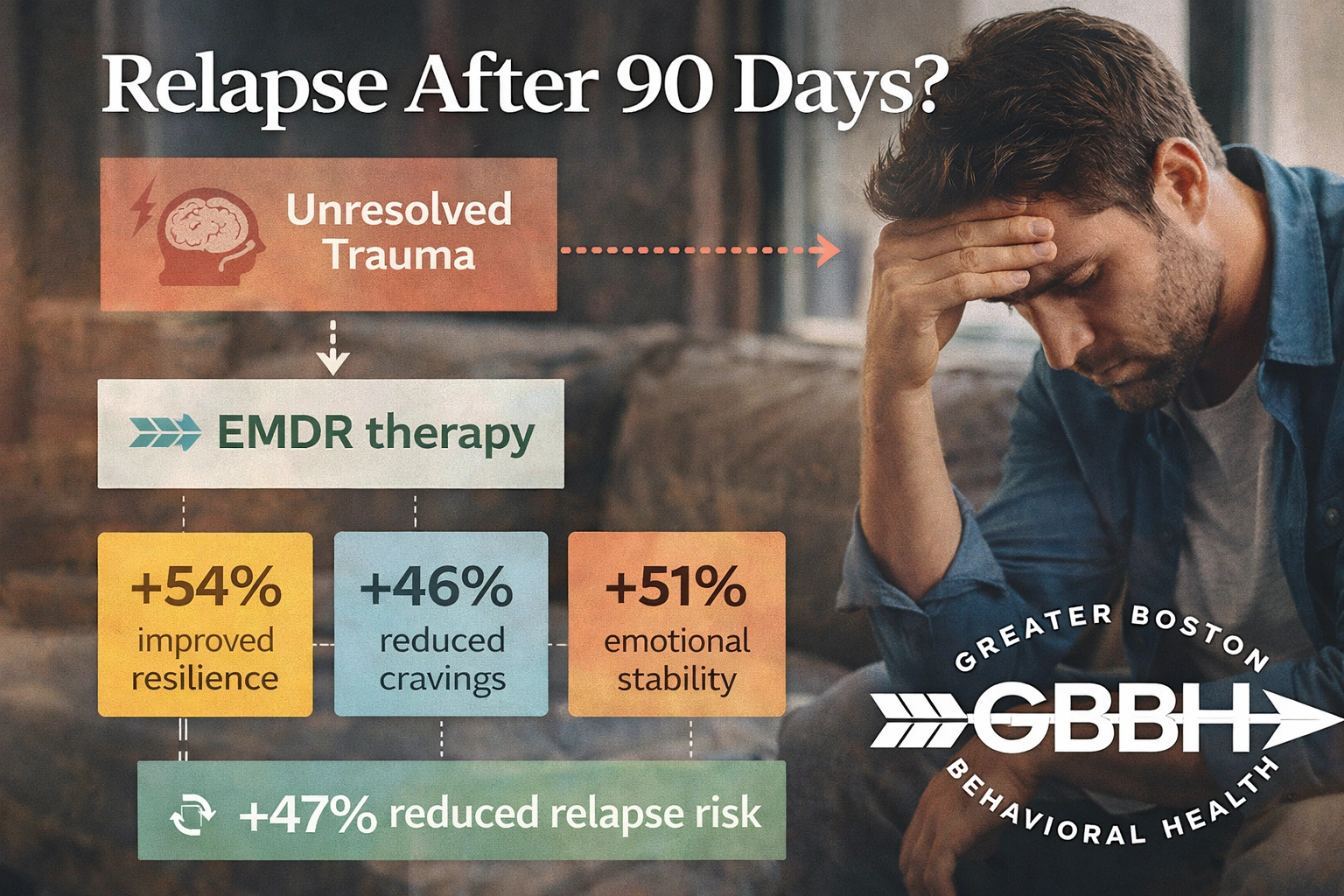
At Greater Boston Behavioral Health, that deeper trauma work includes specialized approaches like emdr, integrated into broader mental health programming. And if you’re near Dedham, Massachusetts, you’re not as far from real support as you might think.
Trauma And Addiction Often Live In The Same House
No one told me early on how often trauma and substance use are connected.
Sometimes the trauma is obvious. Sometimes it’s subtle—chronic stress, emotional neglect, bullying, medical trauma, grief.
Trauma isn’t just about what happened. It’s about what your body learned.
If your nervous system learned that the world isn’t safe, that you’re not safe, that intense emotion equals danger—substances can become a shortcut to relief.
The first time I got sober, I removed the substance.
The second time, I started addressing the alarm system underneath it.
That’s where emdr made the difference.
Healing Trauma Isn’t About Blaming The Past
I used to worry that trauma therapy meant digging up old wounds just to sit in them.
That hasn’t been my experience.
EMDR isn’t about staying stuck in what happened. It’s about updating your brain so it stops responding as if it’s still happening.
There’s a difference between remembering and reliving.
Before, certain triggers would send me straight into survival mode. After several EMDR sessions, those same triggers felt manageable. Noticeable—but not overwhelming.
That shift created space.
And in that space, I could choose differently.
Recovery The Second Time Feels More Honest
The first time, I wanted to prove I could do it.
The second time, I wanted to understand why it was so hard.
That shift in intention changed everything.
I’m not just avoiding substances now. I’m building resilience in my nervous system. I’m challenging old beliefs that quietly shaped my behavior. I’m learning that strength isn’t about pushing through—it’s about processing what you’ve been carrying.
If you’re in the Greater Boston area and close to Needham, Massachusetts, there are accessible pathways to trauma-informed care that weren’t part of your original plan.
You don’t have to settle for repeating the same approach and hoping for a different outcome.
You’re Not Back At Zero
This might be the most important thing I can say.
Relapse does not erase:
- The days you stayed sober
- The skills you learned
- The relationships you built
- The insight you gained
It adds information.
Maybe you learned that stress at work hits harder than you thought. Maybe certain relationships still trigger old patterns. Maybe you realized that coping skills aren’t enough when trauma is unprocessed.
That’s not failure. That’s data.
And data helps you adjust.
What Starting EMDR Actually Felt Like
I expected it to be dramatic.
It wasn’t.
The first few sessions focused on safety, grounding, and identifying targets. My therapist didn’t rush me. We built resources first—internal tools to regulate my body before diving into difficult material.
When we started reprocessing specific memories, I was surprised by how structured it felt. There were clear phases. Clear pacing.
I was never forced to go further than I could tolerate.
After sessions, I sometimes felt tired. Sometimes lighter. Sometimes both.
But over time, the biggest change was this: I stopped reacting to life as if it were an emergency.
And when life doesn’t feel like an emergency, relapse feels less inevitable.
Frequently Asked Questions About EMDR After Relapse
Is EMDR only for severe trauma?
No. EMDR can be used for a range of distressing experiences, from single-incident trauma to chronic stress patterns. If something continues to trigger strong emotional or physical reactions, it may be appropriate to address in EMDR.
Can I start EMDR if I recently relapsed?
It depends on your stability and treatment plan. Many programs integrate trauma therapy once you have enough grounding and support in place. A qualified clinical team can help determine timing.
Will EMDR make things worse before they get better?
Some people experience temporary emotional activation as memories are processed. However, EMDR includes preparation and stabilization phases designed to keep you within a tolerable range. You should feel supported, not overwhelmed.
Do I have to talk about every detail of my trauma?
No. Unlike some traditional talk therapies, EMDR does not require you to describe every detail out loud. The focus is on how the memory is stored and processed internally.
How many sessions does EMDR take?
It varies. Some specific memories can be processed in a few sessions. More complex trauma histories may take longer. Healing is not a race.
What if I tried therapy before and it didn’t work?
Different therapies work differently. If traditional talk therapy didn’t shift the emotional intensity of certain memories, a structured trauma-focused approach like EMDR may offer something new.
If You’re Reading This In Shame
I know that feeling.
The tight chest. The avoidance. The urge to disappear instead of re-engage.
But coming back is not weakness. It’s courage with less ego.
You already know what early recovery feels like. You’ve done hard things before. Now you have more information about what you need.
Maybe that includes trauma processing. Maybe it includes medication adjustments. Maybe it includes stronger boundaries or deeper therapy.
The point isn’t to repeat the exact same path.
The point is to build one that actually supports you.
There Is A Way Forward
Recovery isn’t a straight line. It’s more like learning the terrain of your own nervous system. Sometimes you discover cliffs you didn’t see the first time. Sometimes you find new tools for climbing them.
If EMDR wasn’t part of your first treatment plan, it doesn’t mean you missed your chance.
It might mean you’re ready now.
Call (888) 450-3097 to learn more about our EMDR Therapy in Boston, Massachusetts.