When your child is in crisis, time moves strangely. Every minute feels urgent, yet the path forward can feel paralyzingly unclear. You want to act, but you’re afraid of choosing the wrong thing.
At Greater Boston Behavioral Health, we work closely with parents who are navigating this painful, disorienting space. Many of them are seeking support for a young adult who seems like they’re falling apart—pulling away, breaking down, or slipping into something unrecognizable.
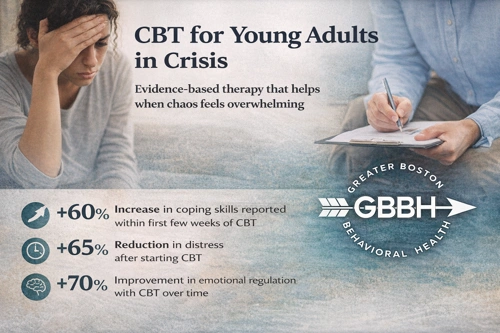
If you’re here, it probably means you’re searching for answers. One approach that continues to offer hope, clarity, and steady progress in the middle of emotional chaos is Cognitive Behavioral Therapy (CBT). In Boston and surrounding communities like Dedham and Needham, CBT is widely used because it helps young people regain a sense of control—often when everything else feels like it’s spinning.
Understanding CBT: Simple Tools for Complex Emotions
CBT stands for Cognitive Behavioral Therapy. It’s a structured, evidence-based form of talk therapy that focuses on how our thoughts, feelings, and behaviors are connected.
But in plain terms, here’s what that means:
CBT helps your child recognize the internal patterns that are keeping them stuck—and teaches them how to interrupt those patterns before they spiral.
This can be especially powerful during a crisis. When emotions are running high, and behaviors are getting riskier or harder to understand, CBT provides a steadying influence. It breaks the cycle of “I feel bad, so I isolate, so I feel worse.” It helps a young person notice that cycle and insert a new choice.
This isn’t magic. It’s a skill. And for many young adults, learning that skill feels like getting the manual to their own mind—something they may never have had.
Why CBT Works During Mental Health Crises
Therapy can feel abstract when a family is in survival mode. You might be asking, “Will this actually help my child right now?”
CBT is one of the most practical, present-focused therapies available. While it absolutely supports long-term healing, it’s also designed to reduce suffering quickly by giving young people something they can do.
That matters. When your child is feeling lost, hopeless, or out of control, action—even small action—can restore a sense of agency.
Here’s how CBT supports recovery during acute moments:
- It teaches emotional literacy. Young adults learn to name what they’re feeling, rather than acting out or shutting down.
- It reduces black-and-white thinking. Instead of “I’m a failure,” CBT helps them say, “I struggled today, but I’m learning.”
- It empowers through choice. Instead of being at the mercy of emotions, they learn how to pause and pick a different response.
- It focuses on now. While trauma-informed, CBT doesn’t require deep dives into the past. It starts with what’s happening today.
That present-moment approach is what makes CBT a safe starting point for so many families in Newton and Waltham.
The Young Adult Brain: Why CBT Fits
Young adulthood is a unique developmental stage. The brain is still forming. Identity is still taking shape. Pressure mounts from school, social life, work, and family.
Add in anxiety, depression, trauma, or other mental health challenges—and things can unravel quickly.
CBT fits the young adult brain because it aligns with how they think and learn:
- It’s concrete rather than theoretical.
- It offers repetition and practice instead of just talk.
- It allows for flexibility and feedback, adapting to what works.
One of our clients from Quincy shared, “I finally had a name for what was happening in my head. I wasn’t broken—I just didn’t know how to respond to myself yet.”
That’s the kind of transformation CBT supports—not through pressure, but through steady skill-building.
When Emotions Are Big and Words Are Hard
Some young adults aren’t ready to “talk it all out.” That’s okay. CBT doesn’t require emotional storytelling to be effective.
In fact, many of the young people we see in our CBT program in Boston, Massachusetts come in guarded, skeptical, or shut down. Their pain is real, but their defenses are high.
CBT respects that. It starts with practical skills. With learning how to track a thought. Or recognize a panic trigger. Or choose a healthier action in a moment of overwhelm.
Over time, that structure often builds trust. It shows the young person that therapy isn’t just about “feelings”—it’s about functioning. And when they start functioning better, the world opens up a little.
What CBT Looks Like in Practice
Here’s a snapshot of what your child might experience in our CBT program:
Initial Sessions:
Their therapist will get to know them, identify current struggles, and begin mapping the patterns that are causing distress.
Middle Phase:
They’ll begin learning specific CBT skills—like cognitive restructuring, behavioral activation, or exposure techniques (if needed). Homework may be given between sessions.
Later Sessions:
Together, they’ll reflect on what’s working, fine-tune their tools, and talk about what sustainable progress looks like.
CBT typically runs for 12 to 20 sessions, but that’s flexible based on the individual. Some young adults continue in CBT while layering in other supports like family therapy, group work, or psychiatry.
For Parents Feeling Powerless: You’re Not
It’s hard to watch your child suffer. Maybe they’re not the same kid you knew a year ago. Maybe their light has dimmed. Or they’ve become angry, avoidant, unreachable.
And maybe you’ve tried other things—school counseling, medication, tough love, gentle talks—and nothing seemed to reach them.
CBT might not fix everything, but it’s a start. A way to reconnect them with their ability to choose something different. A way to stop reacting and start responding.
And that, in a time of emotional crisis, can be the difference between surviving and starting to heal.
You’re not failing as a parent because you don’t have the answers. You’re here, looking for support. That is love in action.
FAQs: CBT and Your Young Adult
Q: Is CBT effective for crisis situations?
A: Yes. While not a substitute for hospitalization during severe crisis, CBT is often used during and after acute periods to help reduce emotional intensity, self-harm, or risk behaviors.
Q: What if my child won’t participate?
A: Many resistant young adults still benefit from the structured nature of CBT. Engagement can start slowly—and often grows as they begin to see results.
Q: Can CBT help with trauma?
A: Yes, especially when integrated with trauma-informed approaches. CBT helps manage trauma responses like intrusive thoughts, hypervigilance, and emotional dysregulation.
Q: Will I be involved as a parent?
A: Yes, if your child consents. We support family communication and will keep you informed about progress and how you can reinforce CBT tools at home.
Q: Is CBT covered by insurance?
A: Often, yes. We can walk you through verification and options based on your specific coverage and needs.
Q: What if my child is already in therapy elsewhere?
A: We can coordinate care or offer a second opinion. Some families use our CBT services alongside other supports.
You don’t have to wait until things get worse. You don’t have to do this alone.
Call (888) 450-3097 to learn more about our CBT services in Boston, Massachusetts. We’re here to help your child feel safe, supported, and capable again—and to help you breathe a little easier, too.