I never thought I’d be the kind of person who went to treatment. I wasn’t falling apart. I had a job. I paid rent on time. I was the one other people leaned on. Sure, I was tired. Sure, I drank a little too much. But I wasn’t one of those people.
Turns out, I didn’t need to be.
What I learned in an Intensive Outpatient Program changed everything I thought I knew about recovery—and about myself.
This is the story of how I stopped waiting for my life to fall apart and started choosing something better.
Rock Bottom Was Never the Goal
For years, I convinced myself I was doing fine. I wasn’t missing work. I wasn’t getting DUIs. I was just tired. Chronically tired. A little numb. Emotionally flat but still functioning.
I told myself: “As long as I don’t hit rock bottom, I’m okay.”
But here’s what nobody tells you—rock bottom isn’t a singular event. Sometimes it’s the slow erosion of joy. It’s the emotional distance you build from your own life. It’s the creeping suspicion that you’re surviving, not living.
I didn’t fall apart. I faded.
And when I finally reached out for help, I realized I didn’t need to be in crisis to need support.
What Made Me Say Yes to IOP
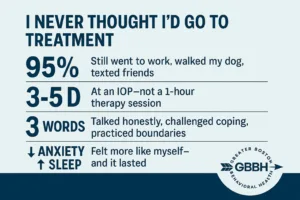
IOP felt like a weird middle ground when I first heard about it. It wasn’t rehab. It wasn’t one-hour-a-week therapy. It was this in-between structure—three to five days a week, multiple hours per day, but no overnight stay.
To be honest, I almost didn’t call. I thought, “I’m not broken enough for something like this.”
But I also couldn’t shake the feeling that I was just… done. Not dramatic, not desperate. Just quietly burnt out. And that was enough.
I reached out. A real person picked up the phone. I cried, hard, after I hung up—not because I was scared, but because it felt like relief.
What Recovery Looked Like in Real Life
I didn’t disappear into a facility. I still went to work. I still walked my dog. I still texted my friends.
But a few mornings a week, I showed up at Greater Boston Behavioral Health’s IOP center and sat in a room with people who got it. Not all of us had the same story—but we all shared that feeling of being secretly not okay.
In group therapy, I learned how to:
- Talk honestly without apologizing
- Challenge my own coping strategies (hello, wine and withdrawal)
- Practice boundaries without guilt
- Feel my feelings without flinching
It wasn’t dramatic. It was steady. It was real. And it helped.
IOP Was Built for People Like Me
High-functioning people often get overlooked in the mental health space. We’re too “together” to raise red flags. But beneath the surface, we’re anxious, exhausted, and spinning inside our heads.
That’s who IOP is for.
It’s not for people who’ve failed. It’s for people who’ve been holding it together for too long.
If you live around Boston—or even nearby in places like Newton, Waltham or Wellesley—IOP gives you a space to reset without stepping away from everything.
You don’t have to lose your job, abandon your family, or explain anything to anyone. You just have to be honest—with yourself, first.
What I Learned That I Never Got from Weekly Therapy
I’d been to therapy before. But it was always once a week, rushed, and surface-level. I’d vent. The therapist would nod. We’d wrap up just as I was starting to say something real.
In IOP, the pace was different. We had time. We built trust. I didn’t just say the right things—I said the hard things.
I also got:
- Peer feedback that felt raw and useful
- Structured exercises that rewired my reactions
- Real-time coaching through triggers
- Group dynamics that broke my isolation
Recovery wasn’t something I thought about once a week. It was part of my life—woven into my mornings, my mindset, my choices.
What Changed (That I Didn’t Expect)
Here’s what surprised me the most:
- I started sleeping. Deeply. For the first time in years.
- I stopped needing a drink to “come down” after work.
- I had energy. Not just fake, performative energy—but real engagement.
- My anxiety went from a constant hum to something I could manage.
- I got my sense of humor back.
These weren’t overnight changes. But they felt real. And they stuck—because I did the work with people who knew what it meant to fake being fine for years.
Signs You Might Be Functioning… But Not Fine
If you’re wondering whether IOP might be “too much” for you, ask yourself this:
- Do you feel emotionally exhausted, even when things are “good”?
- Are you managing stress with alcohol, food, shopping, or isolation?
- Do you hide your real feelings to keep others comfortable?
- Have you convinced yourself this is just adulthood?
- Do you feel like you’re almost okay, but not quite?
If you answered yes to any of those… IOP isn’t too much. It might be just enough.
Frequently Asked Questions About IOP
What exactly happens in an IOP?
You’ll attend structured group sessions (3–5 times per week), engage in evidence-based therapy, and have access to individual counseling. Programs often include CBT, DBT, mindfulness work, and real-world skill-building.
Do I have to stop working to go?
No. Most IOPs—including the one at Greater Boston Behavioral Health—offer flexible scheduling. Evening and morning sessions make it possible to keep your job or care for your family.
Is IOP just for addiction?
Not at all. IOP helps with anxiety, depression, trauma, high-functioning burnout, and more. You don’t need to identify as having an “addiction” to benefit.
How long does it last?
Most programs run between 6 and 10 weeks. The timeline is tailored to your needs, and you’re not locked into anything.
Is it confidential?
Absolutely. Your participation is protected by privacy laws, just like individual therapy. What happens in group stays in group.
What if I’ve already tried therapy and it didn’t work?
IOP is different. It’s immersive. It offers more support, more structure, and more community. If one-on-one therapy felt like not enough, IOP might be the right next step.
Will I be judged?
No. The whole point of IOP is to drop the act. Everyone in the room has their own “I’m fine” mask. The relief of taking it off is mutual.
Final Thought: You Don’t Need a Breakdown to Begin Again
I kept telling myself I wasn’t “that bad.” I waited. I powered through. I tried to white-knuckle my way to wellness.
But you know what? You don’t get bonus points for suffering in silence.
Saying yes to IOP wasn’t a failure. It was the first honest thing I’d done for myself in years.
Ready to Feel More Like Yourself Again?
You don’t have to fall apart to deserve help. If you’re ready to feel better—not just okay—call (888) 450-3097 or visit Greater Boston Behavioral Health’s Intensive Outpatient Program to learn more about services in Boston, Massachusetts.