Premenstrual Dysphoric Disorder (PMDD) is a severe and chronic condition that affects individuals in the luteal phase of their menstrual cycle, typically 7–10 days before menstruation begins. Unlike premenstrual syndrome (PMS), PMDD involves more intense emotional, physical, and behavioral symptoms that disrupt daily functioning and overall quality of life. The condition is classified as a mental health disorder due to its significant psychological impact, including severe mood swings, depression, and anxiety.
For those in Boston, understanding PMDD and accessing effective treatment through behavioral health in Boston or programs like Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs) can be life-changing. This guide explores the types, symptoms, and treatment options for PMDD, along with available resources to help individuals regain control of their mental and physical health.
What is PMDD?
PMDD is a hormone-sensitive mood disorder that typically arises during the second half of the menstrual cycle (luteal phase) and subsides within a few days after menstruation begins. It affects approximately 5–8% of menstruating individuals, significantly impairing daily functioning, relationships, and mental health.
The exact cause of PMDD is not fully understood, but it is believed to involve an abnormal sensitivity to hormonal fluctuations, particularly changes in estrogen and progesterone, which influence neurotransmitters like serotonin. This sensitivity can lead to heightened emotional and physical symptoms.
Symptoms of PMDD
PMDD symptoms are often grouped into emotional, physical, and behavioral categories. These symptoms are more intense and disruptive than those associated with PMS.
1. Emotional Symptoms
- Severe Mood Swings: Intense and unpredictable changes in mood, including episodes of extreme sadness, irritability, or anger.
- Depression or Hopelessness: Persistent feelings of despair, worthlessness, or self-doubt, often resembling symptoms of major depressive disorder.
- Heightened Anxiety: Intense worry or fear, sometimes escalating into panic attacks, requiring intervention through an anxiety treatment program.
- Irritability and Anger: Increased frustration and emotional outbursts that may strain relationships; individuals may benefit from an anger management program to manage these symptoms effectively.
2. Physical Symptoms
- Bloating and Breast Tenderness: Swelling, water retention, and sensitivity in the breasts are common complaints.
- Headaches and Fatigue: Chronic fatigue and migraine-like headaches are prevalent during the luteal phase.
- Changes in Appetite: Intense cravings for specific foods or a complete loss of appetite may occur.
- Sleep Disturbances: Insomnia or excessive sleepiness can significantly impact daily energy levels.
3. Behavioral Symptoms
- Difficulty Concentrating: A reduced ability to focus or complete tasks, often mistaken for attention deficit issues.
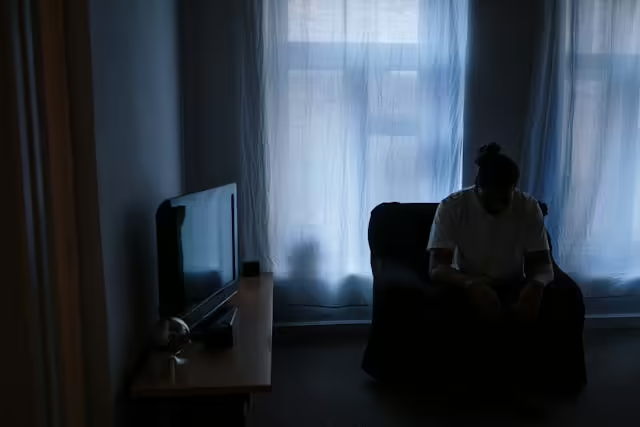
- Social Withdrawal: Avoidance of social situations, work, or family interactions due to emotional instability.
- Impulsive or Self-Destructive Behaviors: Risky actions or self-harm tendencies during peak emotional distress.
How PMDD Differs from PMS
Although both PMDD and PMS occur during the premenstrual phase, PMDD involves far more severe symptoms that interfere with daily life. Understanding these distinctions is essential for accurate diagnosis and treatment.
| Aspect | PMS | PMDD |
|---|---|---|
| Emotional Impact | Mild irritability and mood swings | Severe depression, anxiety, and anger |
| Functional Impairment | Rarely affects daily life | Significantly disrupts daily functioning |
| Duration | Occurs 2-3 days before menstruation | Symptoms last 7-10 days before menstruation |
| Treatment Required | Often managed with self-care | Requires medical and therapeutic intervention |
Risks and Triggers for PMDD
Premenstrual Dysphoric Disorder (PMDD) does not have a single definitive cause, but certain factors can increase the likelihood or severity of its symptoms. Understanding these risks and triggers can help individuals identify potential contributors to their condition and take proactive steps toward managing symptoms.
1. Hormonal Sensitivity
- PMDD is linked to heightened sensitivity to the natural hormonal changes that occur during the menstrual cycle, particularly fluctuations in estrogen and progesterone.
- This sensitivity can disrupt serotonin levels in the brain, leading to emotional instability, anxiety, and depression.
2. Genetic Factors
- Studies suggest a genetic predisposition to PMDD. If a close family member experiences PMDD or other mood disorders, the likelihood of developing PMDD may increase.
3. Mental Health History
- Individuals with a history of depression, anxiety, post-traumatic stress disorder (PTSD), or other mood disorders are at higher risk for PMDD.
- Co-occurring mental health conditions may exacerbate PMDD symptoms, making professional intervention through an anxiety treatment program or depression treatment program essential.
4. Stress and Lifestyle Factors
- Chronic stress can intensify the emotional and physical symptoms of PMDD. Stress also affects hormonal balance, further aggravating symptoms.
- Poor lifestyle habits, such as lack of exercise, unhealthy eating, or irregular sleep patterns, may trigger or worsen PMDD episodes.
5. Substance Use
- Alcohol and drug use can amplify mood swings, irritability, and other PMDD symptoms. Additionally, withdrawal from substances can mimic or exacerbate PMDD-related emotional symptoms.
6. Environmental and Social Factors
- Situational triggers, such as workplace stress, family conflicts, or financial concerns, can heighten the emotional sensitivity of individuals with PMDD.
- Social isolation may also worsen feelings of irritability, hopelessness, or sadness during PMDD episodes.
Treatment Options for PMDD
PMDD is a treatable condition, and effective management often involves a combination of medical, therapeutic, and lifestyle interventions. Below are key treatment options:
1. Medical Interventions
- Selective Serotonin Reuptake Inhibitors (SSRIs):
- Antidepressants like fluoxetine or sertraline can alleviate mood-related symptoms, including depression and anxiety.
- Hormonal Therapies:
- Birth control pills or GnRH agonists can regulate hormonal fluctuations, reducing the intensity of symptoms.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
- Medications like ibuprofen can help manage physical symptoms such as cramps or headaches.
2. Therapy-Based Approaches
Therapy is a cornerstone of PMDD treatment, helping individuals address emotional and behavioral challenges.
- Cognitive-Behavioral Therapy (CBT):
- Focuses on identifying and reframing negative thought patterns, improving emotional regulation.
- Dialectical Behavior Therapy (DBT):
- Helps individuals develop coping mechanisms for emotional distress and interpersonal challenges.
- Anger Management Programs:
- Specifically beneficial for managing PMDD-related irritability and anger, teaching constructive responses to emotional triggers.
3. Structured Mental Health Programs
For those experiencing severe symptoms, structured care options provide intensive and personalized support.
- Intensive Outpatient Programs (IOPs):
- Combine therapy, medication management, and group support in a flexible format, allowing individuals to maintain daily responsibilities.
- Partial Hospitalization Programs (PHPs):
- Offer more intensive care for individuals needing daily therapeutic support without requiring full hospitalization.
4. Lifestyle and Holistic Changes
- Balanced Nutrition:
- A diet rich in complex carbohydrates, lean proteins, and omega-3 fatty acids can stabilize mood and energy levels.
- Regular Exercise:
- Physical activity promotes endorphin release, reducing stress and improving overall mood.
- Stress Management Techniques:
- Mindfulness, meditation, yoga, and journaling help manage emotional and physical symptoms.
Why Seek Help for PMDD?
PMDD is a serious condition that can have a profound impact on physical health, emotional well-being, and daily life. Seeking professional help is essential to manage symptoms effectively and improve overall quality of life.
1. PMDD Impacts Relationships and Daily Functioning
- PMDD can cause severe mood swings, irritability, and depression, often leading to strained relationships with family, friends, and colleagues.
- Social withdrawal and difficulty concentrating can interfere with work, school, or personal responsibilities.
2. Increased Risk of Mental Health Conditions
- Without treatment, PMDD can increase the risk of developing or worsening mental health conditions such as major depressive disorder, generalized anxiety disorder, or PTSD.
- Individuals may experience suicidal ideation during severe PMDD episodes, making timely intervention critical.
3. Challenges of Co-Occurring Conditions
- PMDD often co-occurs with conditions like substance use disorders, eating disorders, or anger management issues. Programs like anger management in recovery or a structured mental health program can address overlapping challenges.
4. Limited Ability to Self-Manage Symptoms
- Self-care practices like exercise or diet changes may not be sufficient for severe PMDD cases. Medical and therapeutic interventions, such as Intensive Outpatient Programs (IOPs) or Partial Hospitalization Programs (PHPs), provide the comprehensive care needed for long-term symptom relief.
5. Improved Quality of Life
- Seeking professional help empowers individuals to manage symptoms, rebuild confidence, and regain control over their lives.
- Tailored treatment plans, including therapy and medication, provide effective strategies for navigating PMDD.
How Greater Boston Behavioral Health Can Help
At Greater Boston Behavioral Health, we understand the challenges of living with PMDD and offer tailored treatment options to help individuals regain control of their lives. Our services include:
- Anxiety Treatment Programs:
Specialized care to address heightened anxiety during PMDD episodes. - Depression Treatment Programs:
Comprehensive support for co-occurring depression. - Anger Management in Recovery:
Learn effective techniques to manage irritability and emotional outbursts. - Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs):
Flexible and structured options for individuals requiring consistent therapeutic care.
Final Thoughts
Premenstrual Dysphoric Disorder is a complex condition that affects millions of menstruating individuals worldwide. Despite its debilitating symptoms, PMDD is highly treatable with the right combination of medical care, therapy, and lifestyle adjustments.
If you or someone you know is struggling with PMDD, it’s important to recognize that you don’t have to face it alone. Professional help can provide the tools, support, and strategies necessary to manage symptoms effectively and restore balance to your life. Resources such as behavioral health in Boston or structured programs like IOPs and PHPs are specifically designed to address the multifaceted challenges of PMDD. Call us today at (888)278-0716 to learn more about our programs and begin your journey toward better mental health.
FAQs on Premenstrual Dysphoric Disorder
How is PMDD different from PMS?
While PMS causes mild to moderate symptoms, PMDD includes severe mood swings, depression, and anxiety that interfere with daily life. PMDD often requires medical and therapeutic intervention.
What are the common symptoms of PMDD?
PMDD symptoms include:
- Severe mood swings and irritability.
- Depression and hopelessness.
- Physical symptoms like bloating and fatigue.
- Difficulty concentrating and social withdrawal.
What causes PMDD?
PMDD is linked to an abnormal sensitivity to hormonal fluctuations, particularly in estrogen and progesterone, which affect brain neurotransmitters like serotonin.
How is PMDD treated?
Treatment options for PMDD include:
- Medical Interventions: SSRIs, hormonal therapies, and pain relievers.
- Therapies: Cognitive-Behavioral Therapy (CBT), anger management programs, and stress management techniques.
- Structured Programs: Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs).
Can lifestyle changes help manage PMDD?
Yes, regular exercise, a balanced diet, and stress management techniques like meditation or yoga can help reduce PMDD symptoms.
Is PMDD a mental health condition?
Yes, PMDD is classified as a mental health disorder due to its significant emotional and psychological impact. It often co-occurs with anxiety and depression.
Where can I get treatment for PMDD in Boston?
Greater Boston Behavioral Health offers tailored treatment options, including anxiety and depression treatment programs, anger management, and structured mental health services like IOPs and PHPs.