When someone first mentioned EMDR therapy to you, your body probably tensed a little.
Maybe your therapist mentioned it as a next step. Maybe you read about it online. Or maybe someone you trust said it “helped them heal their trauma.”
But the second you heard the words “trauma” or “processing,” your chest clenched.
Not because you’re against healing. But because the thought of re-living it—whatever it is—feels like more than you can take right now.
You’ve just been diagnosed. Maybe with PTSD. Maybe with depression. Maybe with anxiety that you’ve been managing on your own for years. And now the idea of going deeper into that pain feels terrifying.
We understand.
At Greater Boston Behavioral Health, we want to say this clearly and compassionately:
EMDR isn’t about reopening old wounds. It’s about helping your brain finally close them—safely, gently, and without re-traumatizing you.
The Misconception: “EMDR Means Re-Living Everything”
This is the most common fear we hear from people who are new to EMDR.
They picture themselves sobbing in a chair, forced to rehash every detail of the worst things that have ever happened. They worry they’ll be made to talk about things they’ve never spoken out loud. They fear losing control—or falling apart completely.
If that’s what you’re imagining, it makes perfect sense that you’re hesitant.
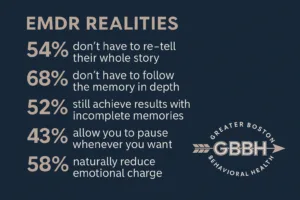
But here’s what’s actually true:
- EMDR doesn’t require you to tell your whole story.
- You don’t have to speak in detail if you’re not ready.
- You’re never forced to “go there” if your body isn’t ready.
- The process is paced with your safety and consent as the priority.
It’s not about flooding you with emotion. It’s about helping your nervous system digest memories that got stuck—so they stop hijacking your present.
What EMDR Therapy Actually Looks Like (and Feels Like)
Let’s take the mystery out of it.
EMDR stands for Eye Movement Desensitization and Reprocessing. That sounds clinical, but the experience is deeply human.
Here’s how a session might go:
- You choose the memory. Not your therapist. You identify something that feels emotionally charged—but not overwhelming.
- You focus on it gently. You don’t have to “relive” it. You just hold it in your mind, like looking at a photo from a distance.
- You engage in bilateral stimulation. This might involve following a light with your eyes, tapping on your knees, or using hand buzzers. It’s not hypnosis. It’s movement designed to help your brain process across both hemispheres.
- Your brain does the work. Images may come up. Emotions may surface. But you are grounded, supported, and always in control.
- The charge lessens. Over time, that memory feels different. Less sharp. Less immediate. Less like it’s happening now.
Some people say it’s like the emotional volume on that memory gets turned down. Others say it’s like their body finally believes they’re safe.
Your Trauma Response Wasn’t a Failure—It Was Protection
You didn’t react “wrong.” You didn’t get stuck because you were weak.
Your nervous system was doing exactly what it was designed to do. Fight, flight, freeze, or fawn—it was all about survival.
But when trauma doesn’t get processed, your brain doesn’t file it away like a past event. It stays present. Active. Triggering.
EMDR helps your brain do what it didn’t get to do before: finish the cycle. Store the memory as something that happened, not something that’s still happening.
It’s not about reliving. It’s about releasing.
You Don’t Have to “Remember It All” for EMDR to Work
Another common fear: “What if I can’t remember what happened clearly?”
That’s okay.
Many trauma survivors have fuzzy, incomplete, or body-based memories. EMDR can work with sensations, emotions, or even images—without a clear narrative.
The brain stores trauma in fragments. EMDR works with those fragments, helping them integrate into a whole. You don’t need to have a perfect story to heal.
EMDR Isn’t Just for Big, Obvious Trauma
You don’t need to have survived a violent event to benefit from EMDR.
People use EMDR to heal from:
- Childhood neglect
- Harsh parenting or emotional invalidation
- Medical trauma or difficult surgeries
- Breakups or betrayals
- Being bullied or excluded
- Ongoing anxiety or panic patterns
- Birth trauma, religious trauma, grief
If something still lives in your body—still sparks dread, shame, or numbness—it’s valid.
If you’re looking for EMDR therapy in Wellesley, MA, our team is trained to work with both “big T” and “little t” trauma—with equal care.
EMDR Is a Structured Process—But You’re Always in Control
This isn’t therapy that’s done to you. It’s a collaboration.
Your therapist won’t rush you. Won’t force you to revisit anything you don’t want to. Won’t assume they know your capacity better than you do.
In fact, many EMDR therapists spend several sessions just building emotional regulation tools before beginning processing.
You’ll learn how to:
- Ground yourself when emotions rise
- Notice when your body is signaling “too much”
- Stay anchored to the present moment
- Use safe “containers” for distressing material
You are not walking into a storm unprepared. You’re being equipped to walk through the past without getting stuck in it.
What EMDR Healing Can Actually Look Like
Some changes are obvious. Others are quiet but powerful.
Clients often report:
- Sleeping better—fewer nightmares or restless nights
- Reacting less strongly to triggers
- Feeling less afraid of being alone with their thoughts
- No longer avoiding certain songs, places, or memories
- A subtle but steady increase in confidence
EMDR doesn’t erase the past. It just helps you stop living in it.
FAQs About EMDR for the Newly Diagnosed
What if I cry or get overwhelmed during a session?
It’s okay to have strong emotions. Your therapist will guide you through regulation techniques and pause if needed. Crying doesn’t mean you’re not coping—it means you’re processing.
Can I try EMDR while I’m still adjusting to a new diagnosis?
Yes. In fact, EMDR can be part of your healing path from the start. Your therapist will assess readiness and tailor sessions to match your emotional capacity.
Will I be “done” with therapy after EMDR?
Not necessarily. EMDR is powerful, but it’s often part of a larger journey. Some people feel significantly better after 8–12 sessions. Others continue in therapy for other goals afterward.
What if I can’t afford long-term therapy?
Ask about sliding scale options, limited-term EMDR intensives, or insurance coverage. Some programs (like ours in West Roxbury, MA) offer short-term EMDR treatment focused on one key issue.
Do I have to stop taking medication if I start EMDR?
No. Medication and EMDR can work together. Always talk with your provider before making any changes.
You’re Not Too Broken. You’re Just Unprocessed.
If you’ve just been diagnosed—or even if you’re still figuring things out—you may feel raw, confused, or fragile.
You might worry you’ll break if you touch the pain.
But EMDR doesn’t ask you to dive headfirst into it. It offers a way to approach gently, with support, and shift the memory from a threat to something bearable. Integratable. Resolved.
Ready to release what you’ve been carrying?
Call (888) 450-3097 to learn more about our EMDR therapy services in Boston, Massachusetts.