Addiction is a complex and multifaceted condition often described as a hijacking of the brain. While this metaphor can be challenging to fully grasp, it effectively communicates the involuntary takeover that compromises decision-making and freedom of choice. Understanding addiction through the lens of brain science reveals how deeply it intertwines with the brain’s natural learning processes, making quitting difficult even when there is a strong desire to do so.
The Role of the Brain in Addiction
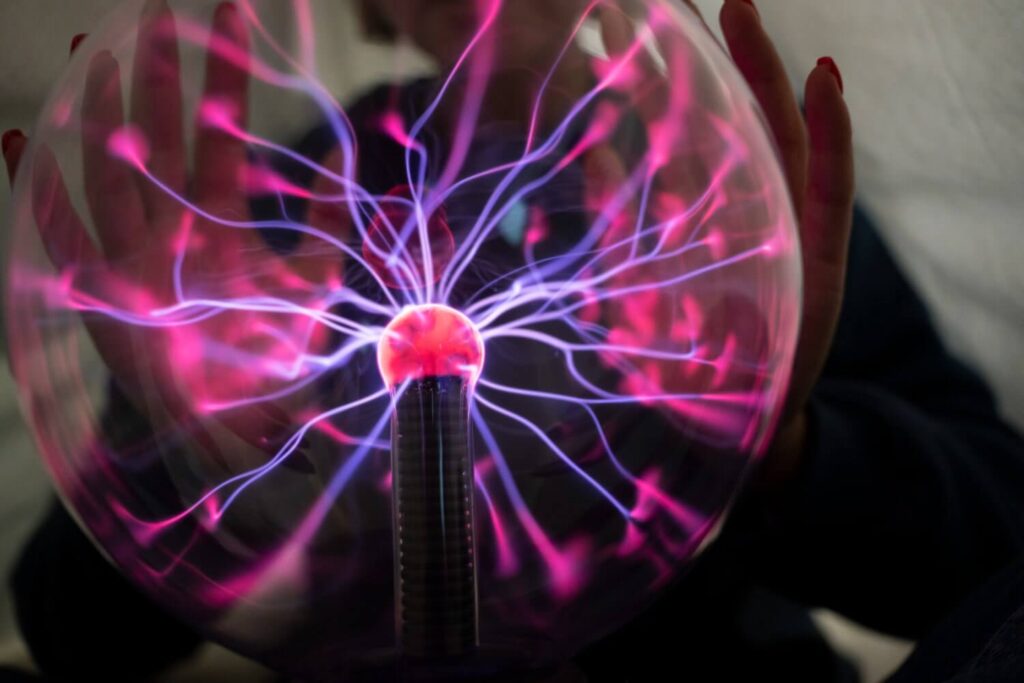
The brain plays a central role in addiction, influencing all human behaviors, including the choice to try a drug. This decision originates in the prefrontal cortex, the brain’s executive center responsible for judgment and impulse control. Once a drug is consumed, it stimulates the nucleus accumbens, a cluster of nerve cells that releases a flood of dopamine, a neurotransmitter often referred to as the “pleasure molecule.”
Dopamine’s role in addiction is rooted in its evolutionary purpose: to encourage repetition of behaviors crucial for survival, such as eating, socializing, and reproduction. Drugs of abuse provide a direct, potent stimulation of this reward system, compelling the brain to seek repeated use.
How Addiction Alters Brain Function
Repeated drug use significantly alters brain wiring, particularly affecting the connection between the nucleus accumbens and the prefrontal cortex. This overactivity weakens the brain’s decision-making capabilities, leading to impaired judgment, reduced impulse control, and a hallmark of addiction: the inability to resist the substance despite negative consequences.
Neuroscience research supports the concept of addiction as a deeply ingrained habit, rapidly rewiring the brain’s circuitry through the power of dopamine. Under its influence, the brain becomes highly efficient at wanting the drug, pruning connections that respond to other stimuli. This biological restructuring explains why addicts continue to pursue drugs, even when aware of the adverse effects.
Is Addiction a Brain Disorder?
Describing addiction as a brain disorder highlights its complexity and subtlety, reflecting the intricate nature of the brain itself. Addiction exploits the brain’s normal pleasure pathways, altering its circuitry in ways that make regulating the allure of drugs increasingly challenging. In response to repeated drug use, neurons become more efficient at relaying signals of pleasure, pruning their ability to respond to other rewards, and weakening connections to impulse control centers.
However, unlike other organ malfunctions, these changes are not biological errors. They represent the brain’s inherent neuroplasticity—its ability to adapt and rewire in response to experiences, which is essential for learning and survival. Recovery from addiction also relies on this neuroplasticity, as changing behavior can rewire the brain toward healthier habits.
The Brain Disease Model of Addiction
The brain disease model of addiction emerged in the 1950s to counteract the perception of addiction as a moral failing. This model views addiction as a chronic condition marked by biological changes in the brain, particularly in the dopamine system, leading to cravings, loss of control, and other dysfunctions associated with substance use. This perspective has led to the development of medications to ease withdrawal symptoms and fostered more compassionate attitudes towards those struggling with addiction.
Despite its benefits, the disease model is controversial. It implies that brain changes in addiction are permanent and that individuals are incapable of overcoming addiction without external help. However, many people successfully quit substance use on their own, suggesting that addiction is not necessarily a lifelong condition. Emerging evidence indicates that the brain changes in addiction reflect normal learning processes, and the brain can return to its baseline state once substance use ceases.
Mental Health Therapy Programs and Addiction
Overcoming addiction often requires more than just stopping substance use; it involves discovering or rediscovering meaningful activities and goals that provide natural and gradual rewards. Mental health programs, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), family therapy, and group therapy, play a crucial role in this process. These therapies help individuals build healthier habits, cope with underlying mental health issues like anxiety disorders, bipolar disorder, and depressive disorders, and develop strategies for maintaining long-term recovery.
How Greater Boston Behavioral Health Can Help
Greater Boston Behavioral Health is dedicated to providing comprehensive support for individuals struggling with addiction through a multifaceted approach that integrates the latest in brain science and evidence-based therapies. By offering a range of mental health therapy programs, including cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and personalized counseling, GBBH helps clients address the underlying issues contributing to their addiction. Call us at – (888) 278-0716 or fill the contact form online.
Our holistic treatment plans are designed to promote long-term recovery by fostering healthier habits, enhancing impulse control, and rebuilding meaningful connections in life. With a compassionate and experienced team of professionals, Greater Boston Behavioral Health empowers individuals to harness their brain’s neuroplasticity, guiding them toward a path of sustainable sobriety and overall well-being.
FAQ on Addiction Through the Lens of Brain Science
What is the role of brain science in understanding addiction?
Brain science helps us understand how addiction affects brain function and structure, revealing the underlying neurological changes that contribute to addictive behaviors. It sheds light on how substances alter brain chemistry and impact decision-making, reward systems, and impulse control.
How does addiction impact brain function?
Addiction can significantly alter brain function by disrupting the brain’s reward system, impairing cognitive functions, and affecting emotional regulation. These changes can lead to compulsive drug-seeking behaviors, reduced ability to experience pleasure, and difficulties in making rational decisions.
What are the key areas of the brain involved in addiction?
The key areas of the brain involved in addiction include the nucleus accumbens, prefrontal cortex, and amygdala. These areas are responsible for reward processing, decision-making, and emotional responses, all of which are impacted by addictive substances.
How does GBBH incorporate brain science into its addiction treatment programs?
At GBBH, brain science is integrated into our addiction treatment programs by employing evidence-based therapies that target neurological changes associated with addiction. We use advanced techniques to understand how addiction affects brain function and tailor our treatments to address these changes effectively.
How does Greater Boston Behavioral Health utilize brain science in their treatment programs?
GBBH incorporates insights from brain science into their treatment programs by using evidence-based approaches that address the neurological and psychological aspects of addiction. Their therapies are designed to support brain health and promote long-term recovery.
How does understanding brain science enhance treatment outcomes at GBBH?
Understanding brain science allows us to design more effective treatment plans by addressing both the biological and psychological aspects of addiction. Our approach helps patients manage cravings, improve cognitive functions, and regain control over their lives, leading to better long-term recovery outcomes.
What makes GBBH approach to addiction treatment unique?
Our approach is unique because we combine cutting-edge brain science research with compassionate care. We integrate this knowledge into personalized treatment plans, ensuring that each patient receives the most effective therapy for their specific needs and brain health.