You look fine.
You still show up. Emails answered. Deadlines hit. Dishes done. On paper, your life makes sense.
So when someone suggests an intensive outpatient program, it almost feels insulting.
But here’s the thing no one tells high-functioning people: the performance can look flawless while the inner life is quietly falling apart.
And if you’re reading this, you probably already know that. You’ve Googled IOPs. You’ve wondered what happens if you stop faking “okay.” You’ve felt the disconnect between being productive and being present.
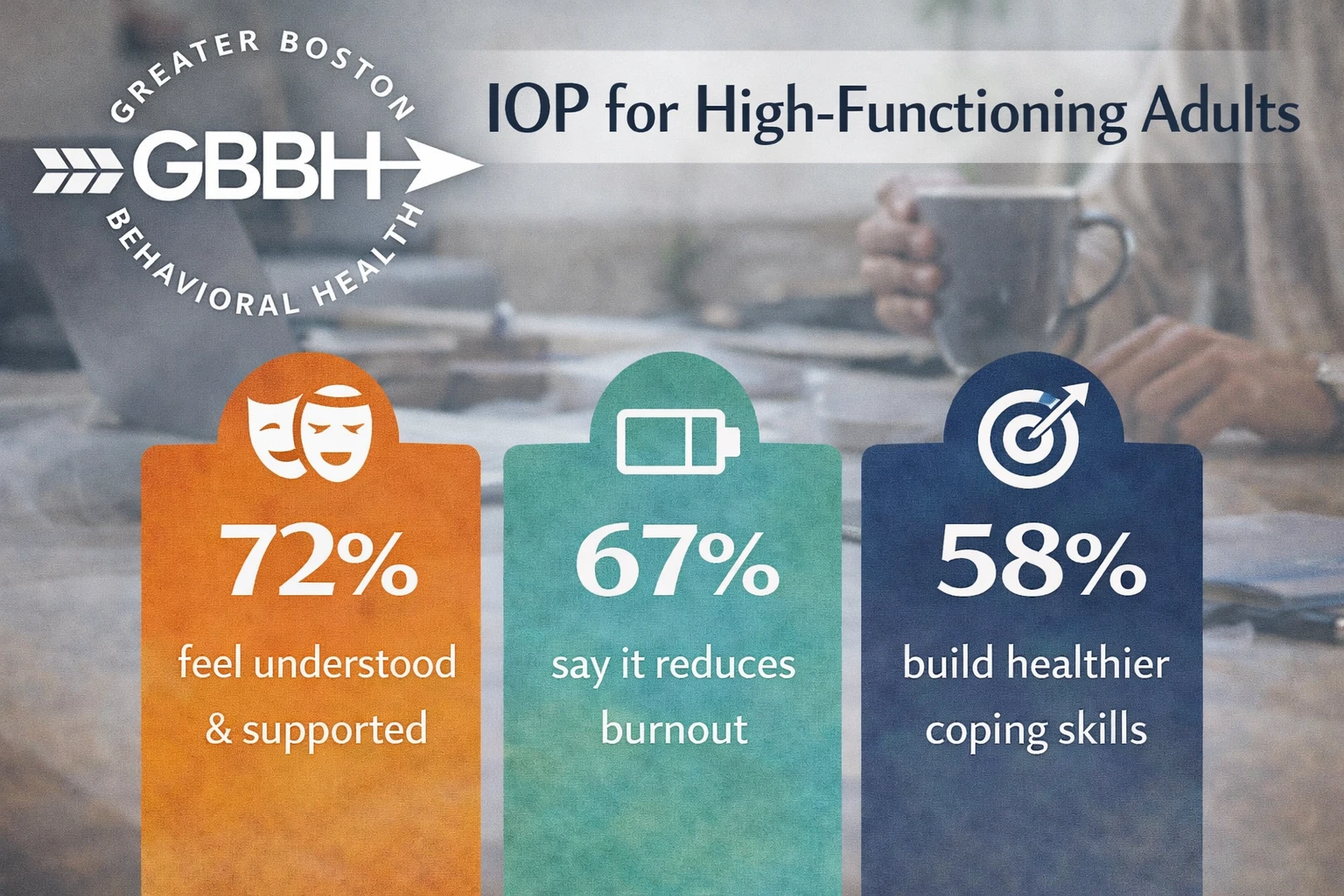
At Greater Boston Behavioral Health, we work with a lot of high-functioning adults. Not because they’re broken. But because they’re tired of carrying the weight of looking fine when they’re not.
Here’s what they don’t expect going in—and what often surprises them most.
You Don’t Have to Be Falling Apart to Need an IOP
High-functioning clients are often their own worst gaslighters.
Because things aren’t visibly chaotic, they assume they don’t “deserve” support.
They tell themselves:
- “It’s not that bad.”
- “I just need to push through.”
- “Other people have it worse.”
But IOP isn’t about extremes. It’s for the gray area.
The space where burnout hides. Where functional addiction thrives.
Where success masks chronic emptiness.
If you’re holding it together—but barely—that’s not strength. That’s strain.
IOP Isn’t a Step Back—It’s a Strategic Recalibration
The idea of entering an intensive outpatient program often triggers fears of regression:
“I can’t do that. I’ve worked too hard.”
“I’m not the type of person who needs that much help.”
Let’s reframe that.
IOP isn’t a breakdown. It’s a strategy.
It offers enough structure to disrupt unhealthy cycles—without removing you from your life.
For many high-functioning people, IOP becomes the first space where they’re allowed to drop the act—and explore the parts of themselves they’ve kept buried under performance, perfectionism, or people-pleasing.
You Might Finally Feel Understood—And That’s the Scariest Part
Here’s the wildest thing we hear:
“I didn’t expect to relate to anyone.”
High-functioning people assume they won’t belong. They fear being the “normal” one in a room full of chaos.
But emotional exhaustion doesn’t care how much money you make.
Burnout doesn’t care if your calendar is color-coded.
Addiction doesn’t skip the accomplished.
When you sit in a room and hear someone say,
“I’m really good at hiding how much I’m hurting,”
it hits different.
Suddenly, you realize you’re not as alone as you thought. And that connection? It changes everything.
CBT and Group Work Hit Different When You’re High-Functioning
A lot of clients have done some therapy before. Maybe even CBT. But in IOP, the pace and purpose shift.
This isn’t about abstract insight or venting for 45 minutes.
This is about learning to actually apply the skills when your thoughts spiral at 2am—or when your emotions shut off at 2pm.
It’s not about saying the right thing. It’s about noticing when you’re running on autopilot—and choosing something different.
In group, something else happens: people start telling the truth. The raw truth. The “I’m exhausted but I’m still performing because I don’t know who I am without being productive” truth.
And for the first time, that honesty gets met with nods. Not silence.
Your Control Patterns Will Be Challenged (That’s a Good Thing)
Control is the safety blanket of the high-functioning.
You’ve built routines, identities, and success on being composed. Reliable. Capable.
But in IOP, the masks come off. Slowly. Gently.
You’re asked questions you haven’t had time—or permission—to ask yourself:
- What’s under the pressure to always get it right?
- Who are you without the overachievement?
- What would it feel like to rest without guilt?
Someone from Needham, Massachusetts once said in group,
“I thought letting go of control would make me spiral. But it actually gave me room to breathe.”
That’s the paradox. Control feels like safety—until it becomes the very thing that’s keeping you stuck.
You Won’t Lose Your Edge. You’ll Learn How to Use It Differently.
This is a real fear: “If I stop pushing myself this hard, will I fall apart?”
The truth? Most high-functioning clients don’t lose their edge—they sharpen it.
Because once you start operating from clarity instead of crisis, your energy gets focused.
Your attention improves.
Your relationships deepen.
Your ambition isn’t just survival anymore—it’s self-directed.
You stop burning fuel just to keep going—and start choosing where you actually want to go.
What You Thought Was Personality Might Be Survival Mode
Maybe you’ve always been “the responsible one.”
The overachiever. The fixer. The go-to.
But what if that identity wasn’t your authentic self—but a response to anxiety, trauma, or fear?
IOP gives you the time and space to ask:
Who am I when I’m not in reaction mode?
That question alone can change your entire relationship to yourself.
A client from Newton, Massachusetts said something that still echoes in our groups:
“I thought I was just intense. Turns out, I was just tired—and never let myself stop.”
FAQs for High-Functioning Adults Considering IOP
Do I have to leave my job to attend an IOP?
No. We offer flexible scheduling—including morning, afternoon, and evening tracks—so you can maintain work, family, or school commitments.
Will I be grouped with people I can’t relate to?
Not likely. We intentionally place clients into programs based on shared experiences, diagnoses, and life circumstances. Many in IOP are just like you: holding it together and questioning how long they can keep doing it alone.
Is IOP therapy every day?
Typically, it’s 3–5 days a week for a few hours each day. That structure is enough to create momentum without overwhelming your life.
What kind of therapy will I get?
You’ll engage in evidence-based modalities like CBT, DBT skills, group process work, and relapse prevention strategies—delivered by clinicians who understand the nuance of high-functioning distress.
How long is the program?
Programs usually last 6 to 12 weeks, with individualized timelines based on your goals and progress.
What if I’ve already tried therapy before?
That’s fine. Many of our IOP clients are returning to therapy after hitting a plateau—or trying to go deeper than what weekly sessions allow.
You don’t need to unravel completely before you seek help.
You don’t need to crash the car to deserve the seatbelt.
An intensive outpatient program doesn’t erase your strength. It redirects it—toward healing, clarity, and a life you don’t have to white-knuckle through.
Call (888) 450-3097 to learn more about our Intensive Outpatient Program (IOP) in Boston, Massachusetts.
If you’re ready to stop performing recovery—and start experiencing it—we’re here.