You’re good at solving problems. Efficient under pressure. Sharp when it counts. On paper, you look fine—even enviable.
So why can’t you exhale?
Why does one offhand comment at work flood you with shame? Why do you jolt awake at 2:17 a.m. with your jaw clenched and your mind sprinting?
This is the paradox we see every week at Greater Boston Behavioral Health: high-functioning, high-performing people who feel like they’re secretly falling apart. And when we introduce EMDR therapy, many finally understand—it’s not about what’s wrong with them. It’s about what their nervous system never got to finish.
High Achievement Doesn’t Cancel Out Unprocessed Pain
We tend to associate trauma with catastrophe—accidents, war, abuse. But trauma can also look like growing up in a house where nobody asked how you felt. Or being praised for your productivity while your anxiety went unnoticed. Or being the caretaker so often that your own needs became invisible—even to you.
When your nervous system is conditioned to brace, appease, or endure, those patterns don’t vanish just because your life looks better now. They adapt. They get quieter. But they’re still running the show.
Here’s how it usually sounds in session:
- “I don’t understand—I have a great job, a stable life. Why can’t I feel calm?”
- “I’ve been to therapy, but I still react like I’m under attack.”
- “Nothing that bad happened. So why does my body feel like it’s always in survival mode?”
Because your body remembers what your brain tries to bury. And you can’t outrun your own biology—not with yoga, not with to-do lists, not with another promotion.
What EMDR Does That Talk Therapy Often Can’t
Talk therapy helps you name patterns. Understand them. That’s valuable. But insight isn’t the same as integration.
EMDR (Eye Movement Desensitization and Reprocessing) taps into how the brain naturally processes memory—especially distressing ones. Through bilateral stimulation (often eye movements), EMDR helps the nervous system reprocess experiences that are “stuck,” so they stop triggering fear, panic, or freeze responses in the present.
It’s like giving your body a chance to refile a memory that’s been left open on your emotional desktop for years.
You still remember what happened. But it doesn’t run you anymore.
Not Every Wound Has a Capital-T Trauma
This is where high-functioning clients often get stuck. They minimize their past because it wasn’t “that bad.” They compare their pain. They use logic to override their body’s signals.
But trauma isn’t about the event. It’s about the response. The moment your nervous system got overwhelmed and couldn’t finish the cycle. The moment you froze, disconnected, or swallowed the scream to survive.
In West Roxbury, Massachusetts, we’ve worked with countless professionals, parents, and overachievers who were shocked by how much their nervous systems were still carrying—quietly, efficiently, painfully.
EMDR gave them a way to stop managing and start metabolizing. To move through what they never got to move out.
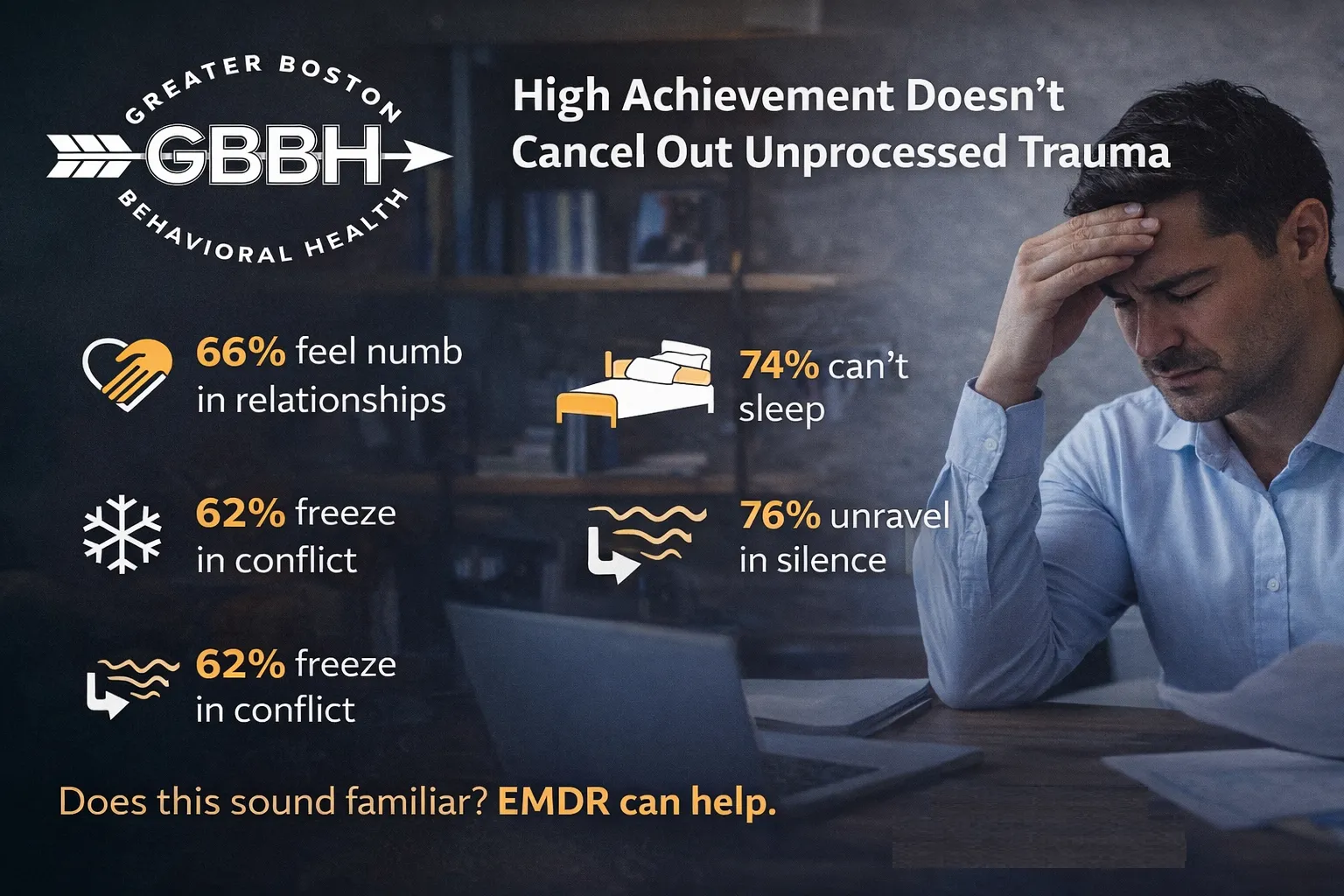
What “Stuck” Can Look Like (Even If You’re High-Functioning)
You may not be melting down or relapsing. But stuck trauma can still show up in your everyday life:
- You’re calm in chaos but unravel in silence
- You freeze in conflict even when you know what you want to say
- You’re exhausted but can’t sleep
- You feel numb in relationships that should feel meaningful
- You constantly brace for impact, even when things are good
This isn’t personality. It’s physiology. And EMDR can help.
EMDR Isn’t Woo-Woo. It’s Brain Science.
Skeptical? Good. You should be.
But here’s the thing: EMDR is recommended by the APA, VA, WHO, and other major organizations for trauma recovery. It’s not fringe. It’s not fluff. And it’s not only for people who’ve been through war zones.
It works because it mimics your brain’s natural processing—specifically, what happens during REM sleep. Those eye movements (or sometimes taps or tones) help both hemispheres of the brain work together to reprocess stuck memories and responses.
It doesn’t erase the past. It takes the charge out of it.
Clients often describe EMDR like this:
“I still remember the event, but it feels… farther away. Like I’m not reliving it every time something reminds me of it.”
That distance? That breathability? That’s the nervous system finally getting to update its files.
Healing Doesn’t Make You Less Capable—It Makes You More Free
A common fear among high-performers is that healing will slow them down. That if they stop running on adrenaline and grit, they’ll lose their edge.
But regulation doesn’t mean deactivation. It means choice.
You’ll still be capable. But you won’t be bracing, scanning, or over-functioning just to feel okay.
In Dorchester, Massachusetts, we’ve seen high-achievers finally allow themselves to rest without guilt. To say no without spiraling. To access deeper creativity, presence, and joy—because their nervous systems were no longer hijacked by old alarms.
That’s not soft. That’s strength, refined.
EMDR Meets You Where You Are—No Need to Perform
You don’t have to come in ready to spill your life story. You don’t need to “believe” in EMDR for it to work. You just need to be open to trying something your body already knows how to do.
At Greater Boston Behavioral Health, our clinicians guide you gently, clearly, and with respect for your pace. You’ll stay in control. You’ll know what’s happening at every step. And you’ll have space to decide when you’re ready to process and when you need to pause.
EMDR isn’t a performance. It’s permission. And most clients find it’s one of the few spaces where their nervous system actually feels safe enough to try something new.
FAQs: EMDR and High-Functioning Clients
I’m not sure I have “real” trauma—can EMDR still help?
Yes. EMDR is effective for chronic stress, emotional neglect, subtle developmental trauma, and any unresolved experience that your body still reacts to.
Will I have to talk in detail about everything that happened?
No. EMDR doesn’t require detailed storytelling. It works with the memory and your body’s response—even without reliving the whole thing.
How long does EMDR take to work?
It depends. Some clients notice a shift in 3–5 sessions. Others need more time. Your clinician will collaborate with you to set a pace that feels right.
What if I’m afraid to feel too much?
That’s normal. We build safety first. EMDR doesn’t flood you. It’s structured, guided, and titrated—so you never go farther than you’re ready for.
Is EMDR covered by insurance?
In most cases, yes. EMDR is a recognized, evidence-based therapy that many plans include. We can help verify your coverage.
If your nervous system is still doing the job it learned years ago—protect, perform, suppress—maybe it’s time to let it retire.
Call (888) 450-3097 to learn more about our EMDR Therapy in Boston, Massachusetts.