There’s a moment—maybe you’ve had it—when your child looks right at you and still feels unreachable. Their eyes are open, but distant. Their answers are short, if they come at all. You don’t know what to say. You’re not even sure what you’re seeing.
But you know something’s wrong.
Whether your young adult has recently enrolled in an anxiety treatment program or you’re just beginning to explore one, you’re likely riding waves of fear, guilt, and confusion. You’re not alone in that. And you’re not a bad parent for not knowing exactly what to do.
At Greater Boston Behavioral Health, we work with families in the thick of this. Not the “before” or the “after.” The middle. The panic. The sleepless nights. The quiet prayers. The “Please let this help.”
This blog is for you—the parent who’s trying to stay steady while everything feels like it’s tilting. Here’s what you can expect when your young adult enters anxiety treatment—and how you can hold on to hope, even when things feel uncertain.
Their Anxiety Isn’t “Just Growing Pains”
If you’ve heard things like, “It’s just stress,” or “They’ll grow out of it,” it’s understandable to feel torn.
But many young adults today are struggling beneath the surface in ways that aren’t visible until they break. Social anxiety. Perfectionism. Panic attacks. Overwhelm that spirals into shutdown. It’s not dramatic. It’s debilitating.
When your child agrees to—or finally accepts—help, it often means they’ve reached their edge. They don’t know what else to do. And neither do you.
That doesn’t mean you’ve failed them. It means they’re hurting. And help is still possible.
Inside a Young Adult Anxiety Treatment Program
So what actually happens once they walk through the doors?
Our anxiety treatment program in Boston, MA is designed to meet young adults where they are—emotionally, developmentally, and psychologically. No lectures. No judgment. Just structure, safety, and steady support.
Here’s what’s typically included:
- Clinical assessment: Before starting, our team conducts a comprehensive review to understand what your child is facing—anxiety symptoms, co-occurring issues, trauma history, and functioning.
- Level of care placement: Based on the assessment, we’ll recommend PHP (Partial Hospitalization Program) or IOP (Intensive Outpatient Program). PHP typically runs 5 days a week for several hours. IOP is a step down—3–5 days per week, shorter blocks of time.
- Individual therapy: Focused sessions where your child builds rapport with a clinician trained in anxiety, trauma, emotional regulation, and young adult development.
- Group therapy: Supervised peer support where your child can hear “me too” for the first time in a while. Sessions often focus on self-worth, coping skills, communication, and anxiety reduction strategies.
- Family involvement: You may be invited into family sessions or coaching—especially if communication has broken down or if your child feels misunderstood at home.
- Psychiatric support (if needed): Medication isn’t required, but for some clients, it’s part of their recovery process. Our psychiatric team helps guide those decisions thoughtfully.
Whether you’re looking for care near Dorchester or West Roxbury, we offer flexible scheduling, virtual options, and integrated services to meet your family’s real-world needs.
It’s Normal If Things Feel Worse Before They Get Better
One of the hardest parts for families is the early phase of treatment—when everything is stirred up, and not much feels better yet.
You might notice:
- Your child is more irritable or shut down.
- They resist going to group or question if this is “working.”
- They start expressing pain they’ve never spoken aloud before.
This is not a sign that treatment is failing. It’s a sign that they’re finally feeling safe enough to let things surface.
Think of it like a fever breaking. The body gets hotter before it begins to heal.
It can be incredibly hard to witness. But it’s also an important turning point.
What You Might Feel as a Parent (And Why You’re Not Alone)
You may feel relieved—and then ashamed for feeling relieved.
You may feel helpless, grieving the version of your child you remember.
You may feel resentment. Guilt. Exhaustion. Hope. All in one day.
These feelings are normal. Parenting a young adult in crisis can leave even the most grounded person feeling unmoored. That’s why we also work with parents—offering space to process what this experience means for you, too.
Your nervous system deserves care. Your story matters in this recovery.
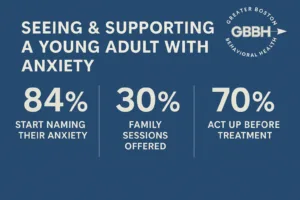
Signs That Treatment Is Helping (Even If It’s Quiet)
Some parents expect big changes—tears of gratitude, emotional epiphanies, apologies. But progress is usually slower. Quieter. More grounded.
Signs treatment is working might include:
- They wake up on time more days than not.
- They start naming their anxiety instead of hiding it.
- They stop avoiding conversations—or start texting back.
- They talk about a group member who helped them feel understood.
- They say “today was okay.”
These are victories. Celebrate them, even if your child doesn’t.
When Success Isn’t Linear (But Still Real)
Relapse is a reality in all forms of behavioral health—not just addiction. Your child may progress, then regress. They may attend consistently for weeks, then skip a session out of fear or fatigue.
This doesn’t mean they’re failing. It means they’re learning what it takes to stay.
Our role is to guide them. Your role is to stay available—not perfect, not all-knowing—just present.
What Success Stories Look Like
You might wonder: Does this actually work?
Here’s what success can look like for young adults who’ve completed our program:
“I didn’t think I’d make it through the first week. Now I’m applying for a job I thought I couldn’t handle.”
– IOP Client, 2023
“My daughter went from hiding in her room to leading a grounding exercise in group. She laughs again. I missed her laugh.”
– Parent, Dedham
“Treatment didn’t fix everything, but it gave my son words for what he’s feeling—and a way to manage it instead of running from it.”
– Parent, Needham
These aren’t miracle stories. They’re human stories. Real, messy, and full of quiet transformation.
FAQ: What Parents Ask Most Often
Q: How involved will I be in the process?
A: That depends on your child’s age, preferences, and treatment plan. For young adults under 26, we often include families in communication, updates, and therapy when clinically appropriate.
Q: What if my child doesn’t want to go—or wants to quit?
A: Resistance is common, especially early on. Our team helps navigate this gently. We support autonomy while reinforcing why they sought help in the first place.
Q: Can treatment help even if anxiety seems like just “who they are”?
A: Yes. Treatment doesn’t erase personality—it helps your child function without being hijacked by fear. Many clients feel more like themselves, not less.
Q: Will they need medication?
A: Not necessarily. Some clients benefit from short-term or long-term medication. Others find relief through therapy and skills alone. We never push—we collaborate.
Q: What happens after the program ends?
A: Discharge planning is part of every client’s treatment. We help transition them to continued care—whether that’s weekly therapy, a support group, or college counseling services.
Call (888) 450-3097 or visit our Anxiety Treatment program in Boston, Massachusetts to learn more about how we support families just like yours. Whether you’re navigating the first call or in the thick of the storm, we’re here—with steadiness, with skill, and with hope.
You don’t have to carry this alone. And your child doesn’t have to fight anxiety in silence anymore. Let’s begin again. Together.