I remember the silence in my apartment after I used again.
Ninety-three days. Gone in one night. No big spiral, no dramatic crash—just me, a locked jaw, and a thousand-pound silence. My first thought wasn’t even “why.” It was, “I ruined it.”
That voice—the one that says you’re back to square one, that nothing counted, that you don’t have it in you to try again—it’s brutal. And it’s wrong.
What helped me challenge that voice and rebuild from the inside out was Cognitive Behavioral Therapy. Not the formal kind you only get in a group room. I mean the tools—the stuff they give you in treatment that we sometimes forget to bring with us after.
CBT became more than a therapy approach. It became my toolkit. My flashlight. My scaffolding. And if you’re here—relapsed, hurting, not sure if you can do this again—it might become yours, too.
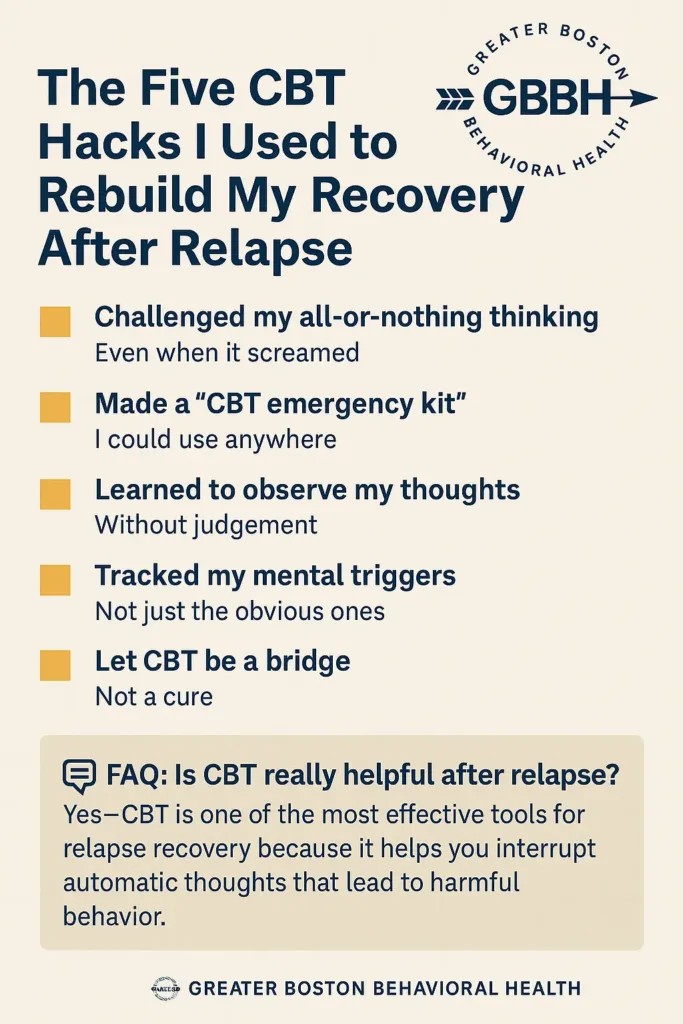
1. I Challenged My All-or-Nothing Thinking (Even When It Screamed)
Relapse feels like a reset button. But here’s the trick my CBT therapist taught me: feelings are not facts.
The morning after I relapsed, my mind said:
- “You lost everything.”
- “You’ll never get 90 days again.”
- “They’re going to be so disappointed.”
Instead of accepting those thoughts as truth, I wrote them down—and challenged them, CBT-style. One by one.
Thought: “You’re back at zero.”
Challenge: “My recovery didn’t disappear. A single slip doesn’t erase my growth.”
Replacement Thought: “I made a mistake. I’m still someone who wants to heal.”
It felt fake at first. But every time I chose a more compassionate reframe, my shame lost just a little bit of power.
2. I Made a “CBT Emergency Kit” I Could Use Anywhere
If you’ve been in treatment, you’ve probably heard someone say “use your tools.” But in early recovery, I didn’t know where to start. So I created a CBT Emergency Kit—a short list of mental go-tos I could pull up fast.
Here’s what mine had:
- 3 grounding statements: “This feeling will pass,” “I’m not my thoughts,” “I’m safe right now.”
- My ‘why’ list: reasons I wanted recovery in the first place (my little brother’s birthday was #1).
- A 3-step check-in: “What am I feeling? What thought is driving it? What action do I want to take?”
I kept it in my phone. Not fancy. Just functional. When I was spinning, it helped me pause, not react.
3. I Learned to Observe My Thoughts Without Judgment
Before relapse, I believed that every negative thought had to be fixed immediately or ignored entirely. CBT taught me a better option: observe without reacting.
Instead of spiraling into “I can’t believe I’m thinking this,” I started saying:
- “Interesting. That thought came up again.”
- “That’s shame showing up. Not the truth.”
- “My brain is trying to protect me with avoidance. But I can choose differently.”
This practice—called cognitive defusion—became my superpower. I could sit with discomfort without letting it drive the car.
4. I Tracked My Mental Triggers (Not Just the Obvious Ones)
The night I relapsed wasn’t random. Looking back with CBT clarity, I saw the setup started days before.
- I skipped therapy.
- I started isolating.
- I told myself I was “fine” because I hadn’t used.
- I believed my low mood didn’t “count” as a threat.
So I started tracking patterns—not just behaviors, but the thoughts that led to them. Some mental triggers I noticed:
- “I don’t want to talk about it” → usually meant I needed to.
- “I’m tired” → often code for emotional burnout.
- “I should be past this by now” → signal of shame creeping in.
Just noticing those thoughts became a form of relapse prevention. I couldn’t always stop the urge—but I could understand where it came from.
5. I Let CBT Be a Bridge—Not a Cure
I wish I could say CBT “fixed” me. It didn’t. But it gave me language. Space. Choices.
CBT didn’t make my cravings disappear. But it gave me the words to describe them to my sponsor. CBT didn’t stop my shame from rising. But it helped me name it, instead of letting it define me.
Here’s the part that’s hard to admit: I wanted healing to feel dramatic. Like a phoenix moment. Instead, it felt like learning to breathe underwater. Slow. Awkward. But possible.
CBT became the bridge between relapse and reconnection. Not a perfect solution—just a path I could walk.
CBT Helped Me Reclaim Recovery—Not Start Over
If you’re sitting where I was—fresh off a relapse, unsure if you belong in recovery anymore—please hear me:
You do.
You are not starting from scratch.
You are starting from experience.
Relapse doesn’t mean the work failed. It means the work is still needed. And tools like CBT don’t just live in therapy sessions. They live in your phone, your journal, your self-talk.
Whether you’re rebuilding quietly or ready to re-engage with support, Greater Boston Behavioral Health is here. Our CBT program in Boston is designed for real life—not perfection. And for those in Needham, Waltham, Newton, or West Roxbury, we have nearby locations to make care accessible.
FAQ: CBT and Relapse Recovery
Is CBT really helpful after relapse?
Yes—CBT is one of the most effective tools for relapse recovery because it helps you interrupt the automatic thoughts that lead to harmful behavior. It’s about building awareness, not shame.
What’s the difference between CBT and just “positive thinking”?
CBT is not about blind optimism. It’s about identifying distorted thinking (like catastrophizing or black-and-white thinking) and replacing it with more accurate, balanced thoughts. It’s practical, not fluffy.
Do I have to be in therapy to use CBT techniques?
While working with a therapist deepens CBT’s impact, you can use many CBT strategies on your own—like thought records, grounding statements, and behavior experiments.
How fast does CBT work?
Some people experience relief within a few sessions, while others take longer. But CBT often helps people feel more in control of their emotions and choices within a few weeks of consistent use.
Can CBT help with the shame I feel after relapsing?
Absolutely. CBT teaches you how to separate feelings from facts. Shame says “you’re broken.” CBT helps you see: “I made a mistake. I can still heal.”
Ready to rebuild—not restart?
Call (888) 450-3097 or visit our CBT services in Boston, Massachusetts. No matter where you’re picking up from, we’re here to walk with you—thought by thought, step by step.